Introduction
The tibial plateau most commonly fractures following high-energy trauma, such as a fall from height or a road traffic accident, from the impaction of the femoral condyle onto the tibial plateau. Less commonly they can occur in elderly patients following a fall, especially those with osteoporosis.
It is typically a varus-deforming force, meaning that the lateral tibial plateau is more frequently fractured than the medial side. They are often found alongside other bony and soft tissue injuries, such as meniscal tears or cruciate or collateral ligament injury.
It is important to recognise that this is a significant injury, as there is disruption of the congruence of the articular surface that, if left, will lead to rapid degenerative change within the knee.
Clinical Features
Patients will present following a history of trauma. A clear history of the mechanism of injury is important, as an injury through axial loading or high-impact injuries will increase the likelihood of a tibial plateau fracture.
Patients will present with sudden onset pain in the affected knee, being unable to weight-bear, and swelling of the knee*.
On examination, significant swelling will be evident, alongside tenderness over the medial or lateral aspects of the proximal tibia, with potential ligament instability (albeit not clinically assessed initially, due to the pain it would cause).
Ensure to check peripheral neurovascular status of the patient, as neurovascular injuries (such as popliteal vessel dissection or common fibular nerve damage) are an important association of high grade injuries.
*This represents a lipohaemarthrosis and is an important clinical and radiological feature to recognise
Differential Diagnosis
For patients presenting with knee pain following trauma, other differentials to consider are knee dislocation, other knee fractures (including patella or distal femur), meniscal injuries, ligamentous injuries, patella dislocation, or patella/quadriceps tendon rupture.
Investigations
The first line investigation for a suspected plateau fracture is plain film radiographs (anteroposterior and lateral), often features on radiograph are subtle (Fig. 2). There will also be a lipohaemarthrosis present.
CT scanning is needed in almost all cases (Fig. 3), apart from undisplaced fractures. This help both in assessment of severity, as well as surgical planning.
*It is important to recognise that the presence of fat in the joint indicates that there is an intra-articular fracture present (e.g. tibial plateau, patella, distal femur)

Figure 2 – Plain radiograph showing tibial plateau fracture
Classification
Tibial plateau fractures can be classified through the Schatzker Classification
| Fracture Type | Description |
| Type I | Lateral split fracture |
| Type II | Lateral split – depressed fracture |
| Type III | Lateral pure depression fracture (rare) |
| Type IV | Medial plateau fracture |
| Type V | Bicondylar fracture (rare) |
| Type VI | Metaphyseal – diaphyseal disassociation |
Table 1 – Schatzker Classification for tibial plateau fractures
Management
Conservative Management
Non-operative management can be trialled in uncomplicated tibial plateau fractures (including no evidence of ligamentous damage, tibial subluxation, or articular step <2mm)
These can typically be treated with a hinged knee brace and non- or partial-weight bearing for around 8-12 weeks, alongside ongoing physiotherapy and suitable analgesia.
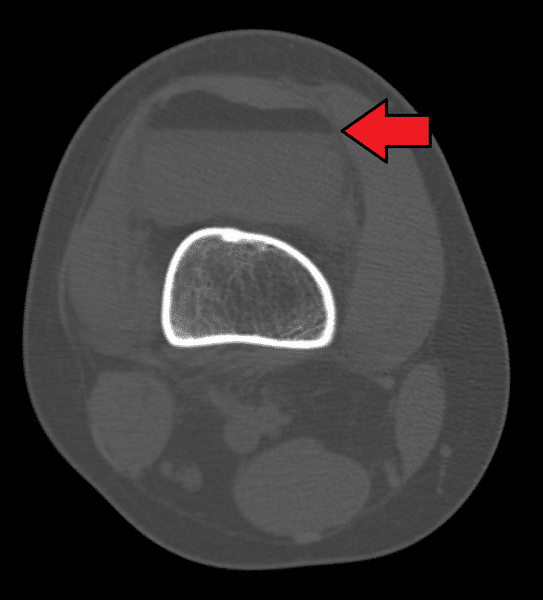
Figure 3 – CT imaging demonstrating lipohaemarthrosis due to a tibial plateau fracture
Operative Management
Operative management is typically warranted in complicated tibial plateau fractures*, or any evidence of open fracture or compartment syndrome. Any form of medial tibial plateau fractures may also require surgical intervention, even if undisplaced, as they have a great potential for displacement.
Open reduction and internal fixation (ORIF) is the mainstay of most tibial plateau fractures, with the aim to restore the joint surface congruence and ensure joint stability. Any metaphyseal gaps can be filled with bone graft or bone substitute.
Postoperatively, a hinged knee brace is fitted with early passive range of movement but limited or non-weight bearing for around 8-12 weeks months is typically required.
External fixation with delayed definitive surgery is indicated in cases of significant soft tissue injury, polytrauma and highly comminuted fractures where an immediate ORIF may not be suitable.
*Complicated fractures include those demonstrating an articular step ≥2mm, angular deformity ≥10 degrees, any metaphyseal-diaphyseal translation, ligamentous injury requiring repair, or those with associated tibial fractures
Complications
The main long-term complication following a tibial plateau fracture is post-traumatic osteoarthritis to the affected joint.
Key Points
- Tibial plateau fractures commonly occur following high-impact trauma
- Ensure to check the neurovascular status of the affected limb
- Initial imaging is via plain radiographs, however definitive treatment often requires CT imaging
- Open reduction and internal fixation is the mainstay of most tibial plateau fractures that require surgery