Introduction
Femoral shaft fractures are common, especially in high-energy trauma, with an incidence of around 4 per 10000 person-years.
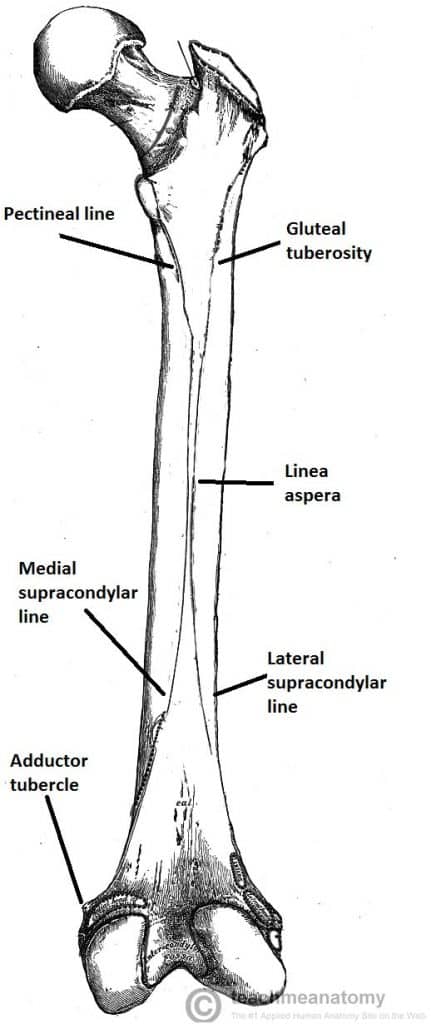
The femur is the longest bone in the body and a highly vascularised bone, due to its role in haematopoesis. The bone is supplied by penetrating branches of the profunda femoris artery, therefore large volumes of blood (up to 1500ml) can extravasate if fractured.
Femoral shaft fractures may be open or associated with neurovascular injury and are most commonly seen in:
- High-energy trauma
- Fragility fractures in the elderly (low-energy trauma)
- Pathological fractures(e.g. metastatic deposits, osteomalacia)
- Bisphosphonate-related fractures*
*Classically this is a transverse fracture in the proximal femur
Clinical Features
The patient will present with pain or swelling in the thigh, hip and/or knee pain, and unable to weight bear. In most cases, an obvious deformity will be apparent from the end of the bed.
Ensure that you assess the skin, which may be open or threatened (tethered, white, non-blanching). The proximal fragment is invariably pulled into flexion and external rotation (by iliopsoas and gluteus medius & minimus, respectively), which can further tent the skin.
Ensure to perform a full neurovascular examination of the lower limbs to check for any vascular or peripheral nerve injury, as well as a thorough secondary survey for associated injuries.
*Referred pain is particularly common in the elderly population with femoral shaft fractures
Classification
The Winquist and Hansen Classification can be used to classify the degree of comminution to femoral shaft fractures:
- Type 0 – No comminution
- Type I – Insignificant amount of comminution
- Type II – Greater than 50% cortical contact
- Type III – Less than 50% cortical contact
- Type IV – Segmental fracture with no contact between proximal and distal fragment
Differential Diagnosis
If the mechanism was high-energy, ensure you perform full ATLS management and formally assess for other injuries. Commonly involved areas that may have fractured include the ankle, tibial shaft, tibial plateau, pelvis, and spinal fractures.
Investigations
Patients presenting following a major trauma should be investigated and managed as per the ATLS protocol.
Routine urgent bloods, including a coagulation and Group and Save, should be sent. Where a pathological cause is suspected, further work-up bloods, such as a serum calcium, may be warranted.
Imaging
A plain film radiograph is the only routine imaging that is often needed (Fig. 2), and should include an AP and lateral of the entire femur, including the hip and knee
Further imaging via CT scanning may be warranted if polytrauma is suspected, to further assess intra-articular or femoral neck fractures.
Management
As per ATLS guidelines, an A to E assessment is vital, stabilising the patient and ensuring appropriate fluid resuscitation.
Ensure the patient has adequate pain relief, often requiring opioid analgesia +/- regional blockade (such as a fascia iliaca block). Open fractures will need to be managed appropriately (discussed here), including antibiotic prophylaxis, tetanus and medical photography.
A femoral shaft fracture requires immediate reduction and immobilisation; reducing fractures to near-anatomic alignment using in-line traction will ensure appropriate haematoma formation and reduce pain.
Most femoral shaft fractures require surgery, however long-leg casts may be indicated in undisplaced femoral shaft fractures in patients not suitable for surgical intervention.
Traction Splinting
Traction splinting, such as a Kendrick traction splint, are used in suspected or isolated fractures of the mid-shaft femur, acting to hold the femur in correct position against action of the large thigh muscle mass.
These are most commonly used in the pre-hospital setting and importantly are not recommended to remain in place any longer than absolutely necessary, due to the risk of skin necrosis at the groin. Traction splints should be changed to skin traction by an orthopaedic specialist as soon as possible.
Contraindications for traction splinting include hip or pelvic fractures, supracondylar fractures, fractures of ankle or foot, or partial amputation.
Surgical Management
Femoral fractures should be surgically fixed within 24-48 hours, although sooner if an open fracture.
Most isolated cases can be treated with an antegrade intramedullary nail*, which have around a 98% union rate and a low rate of post-operative complications.
External fixation (with subsequent delayed conversion to intramedullary nail) may be used in unstable polytrauma or open fractures, to ensure the patient is physiologically optimised prior to definitive fixation.
*A retrograde intramedullary nail may be used if the femoral fracture is more distal or if the patient has an ipsilateral hip replacement
Complications
Common complications following femoral shaft fracture include:
- Nerve injury or vascular injury
- Pudendal nerve injury (around 10%) or femoral nerve injury (rare)
- Mal-union (or rotational mal-alignment), delayed union, or non-union
- Mal-union occurs in around 30% and 10% of proximal and distal fractures respectively
- Infection, especially with open fractures
- Fat embolism
- Venous thromboembolism
More long-term problems include hip flexor or knee extensor weakness, limb stiffness, or re-fracture.
Prognosis
Patients who survive the initial trauma associated with the injury typically heal well.
Early mobilisation following surgical intervention greatly reduces complications. Bilateral femur fractures have higher rates of pulmonary complications and increased mortality rates, compared to unilateral fractures.
Key Points
- Femoral shaft fractures are common, especially in high-energy trauma or as pathological fractures in the elderly
- Patients present usually following trauma, with pain in the thigh and unable to weight bear
- All suspected cases require a plain film radiograph, both lateral and AP views
- Most cases will require surgical management, with most isolated cases treated with an antegrade intra-medullary nail