Introduction
Carcinoma of the breast is the most common cancer in the Western world and accounts for 30% of new cancer diagnoses in women in the UK. The lifetime risk of breast cancer in the UK is 1 in 7 in females (the prevalence of the condition in males is significantly less).
Invasive carcinoma of the breast can be classified* into:
- Invasive ductal carcinoma (70-80%)
- Invasive lobular carcinoma (5-10%)
- Other subtypes, such as medullary carcinoma, invasive micropapillary carcinoma, or metaplastic carcinoma
*Historically, ductal and lobular carcinomas were originally divided on the basis that ductal carcinomas arise in the ducts and lobular carcinomas arise in the lobules; it is now known that almost all breast carcinomas actually arise in the terminal duct lobular unit but this classification remains in use due to the different behaviour of the two subtypes.

Figure 1 – macroscopic appearance of breast carcinoma, following simple mastectomy
Classification
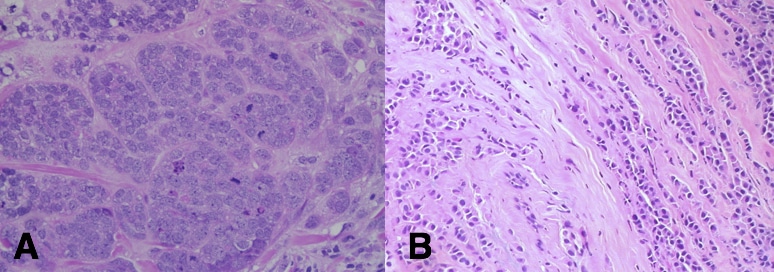
Invasive ductal carcinoma (IDC) is the most common type of breast carcinoma, constituting 70-80% of all cases. Microscopically, IDC is composed of nests and cords of tumour cells with associated gland formation.
Invasive lobular carcinoma (ILC) is the second most common type of breast cancer, constituting 5-10% of all invasive breast cancers and is more common in older women. It is characterised by a diffuse (stromal) pattern of spread that makes detection more difficult. By the time of diagnosis, tumours can often be large.
Risk Factors
Female sex and increasing age are the most significant risk factors for breast cancer, with the disease is 100x more common in women, whilst age-associated risk in women doubles approximately every ten years until the menopause (the risk then plateauing after 75-80yrs)
Family history of breast cancer can be a significant risk factor. Less than 10% of all breast cancers are linked with a genetic mutation. Breast cancer susceptibility gene 1 and 2 (BRCA1 and BRCA2) are the commonest breast cancer associated gene mutations; these genes increase breast cancer risk from between 45-70%, as well as increase the risk of ovarian, prostate, and pancreatic cancer.
Degree of exposure to unopposed oestrogens has also been well-documented to cause an increase in risk to develop breast cancer. Factors that influence this include early menarche, late menopause, nulliparity, and long term (5 years or more) use of Hormone Replacement Therapy (often used for managing menopausal symptoms).
Previous benign breast disease, obesity, alcohol consumption, smoking and geographic variation (more common in developed countries) are all associated risk factors for breast malignancy.
Clinical Features
Patients can present symptomatically or asymptomatically via screening.
Clinical features may include breast or axillary lump(s), asymmetry, or swelling, abnormal nipple discharge, nipple retraction, skin changes (dimpling/peau d’orange, or Paget’s-like nipple changes) and mastalgia.
Differential Diagnosis
The symptoms and signs described above can be a result of both malignant or benign pathology. Benign breast lumps, cysts, or infection are all possible non-malignant differentials. Any symptoms that raise suspicion of breast cancer should be referred for a triple assessment.
Investigation and Management
The current gold standard for diagnosis of breast lumps is via triple assessment. This comprises examination, imaging with mammography and ultrasound (MRI is used in a minority of cases), and biopsy.
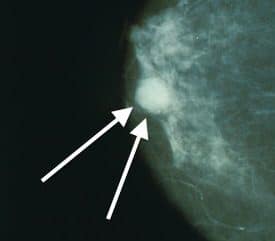
Figure 4 – A mammogram demonstrating a breast cancer (arrow)
Following triple assessment and the diagnosis of breast cancer, management is determined by a Multi-Disciplinary Team (MDT). This comprises breast surgeons, oncologists, radiologists, histopathologists and breast care nurses.
Treatment options are comprised of surgery, radiotherapy, chemotherapy, hormonal therapy, and / or antibody therapy. The combination of which treatments recommended are based upon tumour stage, biology and patient factors (frailty comorbidity etc). Further detail on breast cancer management is available here.
Prognosis
Breast cancer prognosis is influenced by nodal status, size, grade, and receptor status.
The Nottingham Prognostic Index (NPI)* is a widely used clinicopathological staging system for primary breast cancer prognosis. It is calculated by:
(Size x 0.2) + Nodal Status + Grade
Size is the diameter of the lesion in cm, nodal status is number of axillary lymph nodes involved (0 nodes=1, 1-4 nodes=2, >4 nodes=3), and the histological grade is based on Bloom-Richardson classification
| Score | 5 Year Survival |
| ≥2.0 and ≤2.4 | 93% |
| >2.4 and ≤3.4 | 85% |
| >3.4 and ≤5.4 | 70% |
| >5.4 | 50% |
*Importantly, this data was first published in 1992 and a variety of other factors, outside of the NPI, such as vascular invasion and receptor status, are now also used in prognostics
All breast malignancies are checked for their expression of Oestrogen Receptor (ER), Progesterone Receptor (PR), and Human Epidermal growth factor Receptor (HER2). The presence or absence of these receptors determines suitability of targeted adjuvant therapies (including endocrine and monoclonal antibody therapies).
The pattern of receptor expression (and the broader treatment options available in receptor positive disease) has implications on cancer prognosis. Tumours that are negative for all three receptors are associated with a poorer prognosis.
Breast Screening Programmes
In the UK, the NHS breast cancer screening programme currently invites women aged 50-71yrs to have a mammogram every three years; any abnormalities identified will be referred to breast clinic for triple assessment.
Paget’s Disease of the Nipple
Paget’s disease of the nipple is a rare condition, presenting as a persistent roughening, scaling, ulcerating or eczematous change to the nipple. The vast majority of Paget’s (85-88%) will also have an underlying neoplasm, either in-situ or invasive disease, and it is associated with 1-3% of all cases of breast cancer.
Microscopically there is involvement of the epidermis by malignant intraepithelial adenocarcinoma cells within the nipple epidermis. The mechanism behind Paget’s disease is currently unknown, however it is hypothesised that either malignant cells migrate from the ducts to the nipple surface or the cells of the nipple themselves become malignant
Clinical Presentation
Clinical features for Paget’s disease of the nipple include an itching or redness in the nipple and/or areola, with flaking and thickened skin on or around the nipple (Fig. 5).
The area is often painful and sensitive. A flattened nipple, with or without yellowish or bloody discharge, may also be indicative of the disease.

Figure 5 – Paget’s Disease of the Nipple, involving the areola and the nipple
Differential Diagnosis
Due to its involvement of the skin of the nipple, Paget’s disease of the breast is often mistaken for dermatitis or eczema.
Paget’s disease can be differentiated from eczema on the basis that the former always affects the nipple and only involves the areola as a secondary event, whilst eczema nearly always only involves the areola and spares the nipple.
Investigations and Management
A biopsy is needed to confirm diagnosis. Given its association with malignancy, a complete breast and axilla examination should also be performed; mammograms, ultrasounds, or MRI breast may also be warranted.
First line management of Paget’s disease is operative, if possible. The type of surgery depends on how advanced the underlying breast cancer is, but in all cases the nipple and areola will need to be removed. In the cases associated with an underlying malignancy, radiotherapy may also be necessary.
Key Points
- Most invasive breast cancers are either ductal carcinomas or lobular carcinoma
- Wide array of presentations, any suspected case should be sent for triple assessment
- A range of management options for breast cancer are available
- The Nottingham Prognostic Index (NPI) is a clinicopathological staging system used for primary breast cancer prognosis