This article is for educational purposes only. It should not be used as a template for consenting patients. The person obtaining consent should have clear knowledge of the procedure and the potential risks and complications. Always refer to your local or national guidelines, and the applicable and appropriate law in your jurisdiction governing patient consent.
Overview of Procedure
There are several types of abdominal hernia, the most common being inguinal, femoral, and umbilical.
Inguinal hernia repairs are of the following three general types:
- Herniotomy – removal of the hernial sac with ligation and excision of the patent processus vaginalis, most commonly performed in neonates/ infants
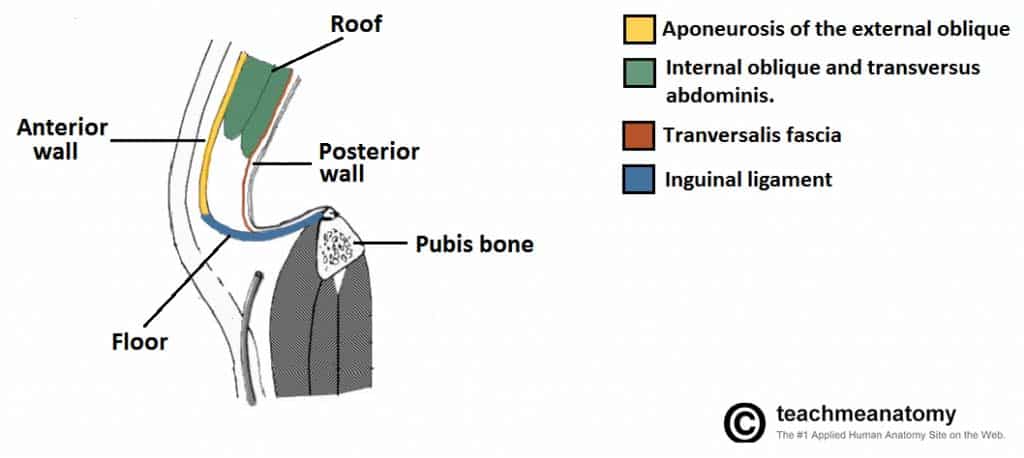
- Herniorrhaphy – herniotomy with suture repair of the posterior wall of the inguinal canal
- Hernioplasty – herniotomy with reinforcement of the posterior wall of the inguinal canal with a synthetic mesh
For an open inguinal hernia repair, the inguinal canal is opened, the cord structures separated from the hernia sac, and the hernia sac ligated and reduced. A mesh is typically placed on the posterior wall of the canal and the canal then closed. The most common technique is the Lichtenstein tension-free mesh repair.
Complications
Intraoperative
| Complication | Description of Complication | Potential Ways to Reduce Risk |
| Haemorrhage | Injury to inferior epigastric, external iliac, and/or femoral vessels | Avoid taking deep bites when suturing the mesh medially onto the inguinal ligament, to avoid underlying femoral vessels |
| Injury to surrounding structures including bowel, bladder, spermatic cord (vas deferens) | Contents of the hernial sac may include these structures and in a sliding indirect inguinal hernia they can form part of the wall of the sac | |
| Bowel resection | Incarcerated hernias may contain ischaemic bowel; if the bowel is not viable it must be resected | |
| Anaesthetic Risks | Includes damage to the teeth, throat and larynx, reaction to medications, nausea and vomiting, cardiovascular and respiratory complications | Forms a part of the anaesthetist assessment before the operation |
Early
| Complication | Description of Complication | Potential Ways to Reduce Risk |
| Pain* | Injury to the ilioinguinal and/or genitofemoral nerves
Chronic pain from anchoring sutures in mesh repair |
Avoid taking deep bites through the periosteum of the pubic tubercle
Attempt to preserve the ilio-inguinal nerve; if not feasible, resect it proximally to avoid risk of being trapped during the repair |
| Loss of sensation | Damage to ilioinguinal and/or genitofemoral nerve | |
| Bleeding/ haematoma | There is a small chance of bleeding and bruising in the abdomen post-surgery. | Ensure appropriate ligation of vessels and good haemostasis at every stage of the procedure |
| Infection | Superficial wound infection is possible. An infected mesh is a fortunately rare but serious complication, as would be revision of wound | Peri-operative antibiotics will reduce the risk of wound infections |
| Scarring | Any incision will result in a scar, which may form a keloid scar, particularly in high risk ethnicities. | |
| Seroma | A swelling of lymphatic fluid may occur in redundant subcutaneous space following surgery. | |
| Blood Clots | DVTs and PEs are a possibility in any operation. The risk is increased in patients with a raised BMI, on the pill, recent flights, previous DVT, pregnancy, smokers, cancer and prolonged bed rest. | The patient will be given anti-embolism stockings and low molecular weight heparin peri-operatively to minimise this risk as deemed appropriate. |
| Testicular Atrophy | Damage to the blood supply to the testicle can occur in groin hernia repair, often due to venous thrombosis rather than arterial injury | Identify and avoid damage to the spermatic cord and associated vessels |
| Scrotal swelling or hydrocoele | Damage to venous/ lymphatic drainage during dissection | |
| Stroke, MI, Kidney Failure, Death | Although small, this is always a risk in any major surgery |
*Patients may have long-standing pain from hernia pre-operatively. Importantly, for inguinal hernias, 1 in 50 patients have severe long-standing groin pain post-operatively and 3 in 50 are symptomatically worse than they were before the operation, hence this is very important to discuss and explicitly consent for.
Late
| Complication | Description of Complication | Potential Ways to Reduce Risk |
| Recurrence | There is always a potential for further surgery due to recurrence of the hernia. Rates vary between procedures: for inguinal hernia it is around 1% at 5 years. | Request the patient avoids strenuous activity for a few weeks post-operatively |