Introduction
Flexor tendon injuries are rare, however can be serious when they do occur. They typically result from a traumatic injury, such as a laceration to the volar hand surface, and therefore can occur with concurrent neurovascular injury.
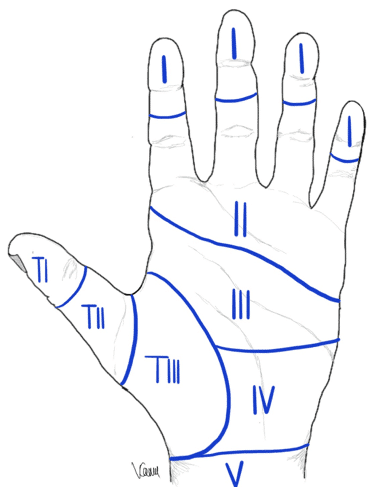
Any flexor tendon hand injuries are classified based on Verdan’s zones (Fig. 1). They are important to determine in any suspected tendon injury, as they affect management and overall prognosis. Broadly, they can be divided into:
- Zone 1 – Flexor Digitorum Profundus only
- Zone 2 – Flexor Digitorum Superficialis and Flexor Digitorum Profundus
- Zone 3 – Central palm (from the carpal tunnel to distal palmar crease)
- Zone 4 – Carpal tunnel
- Zone 5 – Proximal to carpal tunnel
- Thumb – Specific to the thumb
Hand Flexor Anatomy
The flexor tendons found in the hand are Flexor Digitorium Profundus (FDP), Flexor Digitorium Superficialis (FDS), Flexor Pollicis Longus (FPL), Flexor Carpi Radialis (FCR), and Flexor Carpi Ulnaris (FCU). Blood supply to the flexor tendons come from two sources, direct vascular perfusion and diffusion through synovial sheaths.
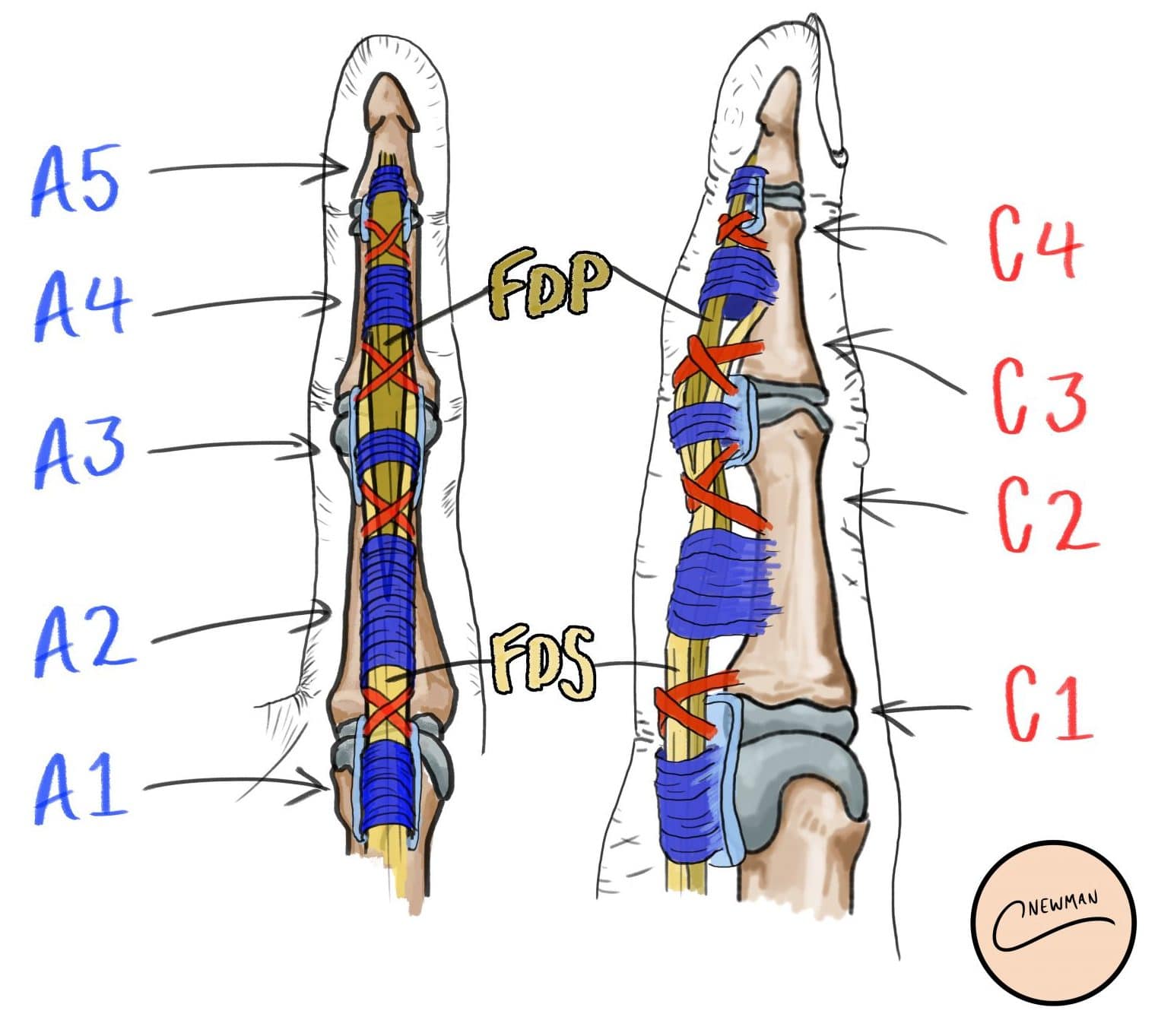
These tendons are kept in place (preventing bowstringing) via use of a series of pulleys. Digits 1-4 contain 5 annular pulleys*, labelled A1 to A5, and cruciate pulleys, labelled C1 to C4 (Figure 2). The thumb contains two annular pulleys and one interposed oblique pulley.
*A2 and A4 arise from the bone, whilst A1, A3, A5 arise from the volar plate
Clinical Features
Flexor tendon injuries commonly occur following penetrating trauma to the arm, hand or fingers, however can also occur with contact sports or exercises, such as rugby or rock climbing.
Following the initial injury, the patient will report, to varying degrees, an inability to flex their finger(s); complete injuries will present as an inability to move that joint, but partial injuries may present with weakness or pain on resisted movement.
Tendon injuries may not always be visible through any wound present, therefore it is important to inspect the hand characteristics at rest* (see Examination of the Hand). Ensure to assess for any neurovascular compromise.
Passively extend the patients wrist whilst asking them to relax their upper limb fully and this will allow assessment of the tenodesis effect; maintenance of digit extension at the proximal interphalangeal joint (PIPJ) or distal interphalangeal joint (DIPJ) with wrist extension indicates a fault with the flexor tendon.
*In flexor tendon injuries, the affected phalanx may be in extension, in comparison to other non-affected digits, either at rest or on specific movement
Investigations
All suspected tendon injuries should have a plain film radiograph of the affected hand, to exclude any underlying fractures and foreign bodies.
Whilst the diagnosis of flexor tendon injuries is typically clinical, ultrasound imaging can be used to confirm the diagnosis in a small amount of cases (this would need to be performed by a MSK radiologist and is very operator dependent).
Management
Following initial injury, all jewellery must be removed and any wound present irrigated to reduce any gross contamination. A tetanus booster should be given (if status is uncertain) and antibiotics started. Keep the hand elevated to reduce swelling.
Most wounds with a suspicion of flexor tendon injury will undergo exploration +/- tendon repair and washout in theatre, before being closed and placed in a splint.
A small proportion may have non-operative management, however this risks future trigger finger development. In such cases, early mobilisation and rehabilitation with hand therapists is important to preserve the strength and the digit function.
Operative Management
Any operative technique should be determined on a case by case basis. Whilst no definitive criteria, flexor tendon repairs are often performed in those with >50% laceration (or less in cases of triggering). This can be done under general anaesthesia or with a regional block.
Flexor tendon reconstruction is an alternative option, whereby either the palmaris longus, plantaris, or extensor digitorum longus (to 2nd-4th toes) tendons are used as grafts
Prognosis
Improved compliance with post-operative controlled mobilisation has led to significantly improved outcomes to tendon repairs in recent years.
Complications that can occur include tendon adhesions, bowstringing, re-rupture (~20% lifetime risk), joint contracture, swan-neck deformities, and trigger finger.
Key Points
- Flexor tendon injuries typically result from a traumatic injury
- Patient will report, to varying degrees, an inability to flex their finger, and the diagnosis is often clinical
- Most cases with a suspicion of flexor tendon injury will undergo exploration +/- tendon repair and washout in theatre