Introduction
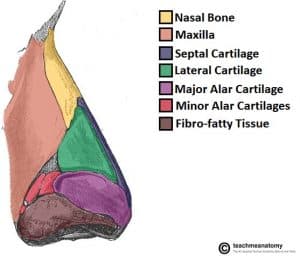
Nasal trauma is a common injury and can result in varying amounts of damage to any of the component structures, including the skin, the cartilage, or the bone.
As with any trauma, initial assessment of facial trauma should always be performed as per standard ATLS protocol. Nasal injuries may be isolated or co-exist with other injuries, such as naso-orbital-ethmoid fracture, or maxillary fracture especially if there was high impact facial trauma. These will take priority over the nasal injuries.
However, the majority of nasal fractures are isolated injuries. As a generic approach to any nasal trauma, it is important to establish the mechanism of injury; including impact, force, direction and timing. Key symptoms to enquire about include pain, nasal deviation, obstruction, discharge, and epistaxis; examination of the nose can be found here.
This article will focus specifically on isolated nasal trauma.
Nasal Laceration
Nasal skin lacerations can often be difficult to manage due to the 3-dimensional complexity of the nose shape.
The wound should be cleaned* and, where possible, the skin edges opposed. This can be done with either steri-strips or sutures. If primary closure is not possible, referral to plastic surgery or ENT may be required (or left to heal by secondary intention, but will have undesirable scarring).
Occasionally, if there is displaced nasal bone fracture that is preventing the wound from being opposed, the fracture will need to be reduced under anaesthetic prior to primary closure of the laceration. This should be done urgently as it is considered an open fracture.
*Consideration should also be given to tetanus prophylaxis, depending on the mechanism of injury and the vaccination status of the patient; patients will also need to be started on oral antibiotics as there was an open wound
Septal Haematoma
Septal haematoma is an important finding that should not be left out in the initial examination of a patient with nasal injury, as can be serious if left untreated.
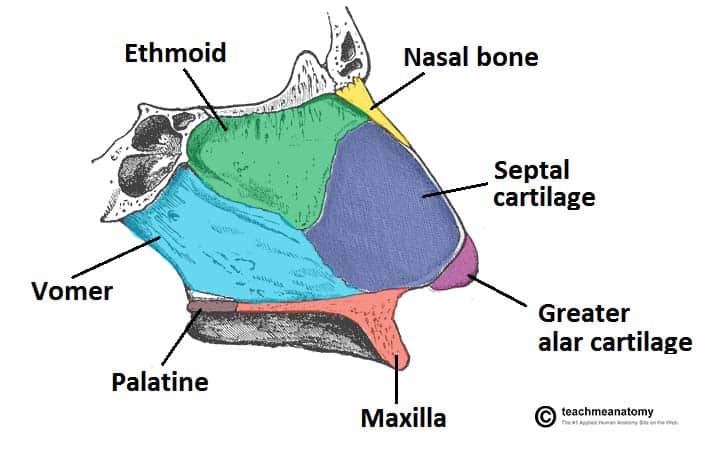
A septal haematoma will develop following trauma, whereby the shearing forces involved result in a separation of overlying perichondrium from the nasal septal cartilage. This causes submucoperichondrial blood vessels to tear and blood to accumulate within this space.
Septal haematomas are visible on anterior rhinoscopy as a boggy red/purple swelling from the nasal septum (Fig. 2). Using a Jobson Horne probe, gently palpate the mucosa, as a haematoma will be fluctuant, which helps to differentiate from a deviated septum (normally unilateral).
Treatment involves incision and drainage of the haematoma, usually under general anaesthetic. Proper quilting sutures will need to be done to ensure there no recurrence of haematoma; this is often supplemented with the use of nasal splints bilaterally, which are removed after 1 week.

Figure 2 – Bilateral septal haematoma in a 5yr old following nasal trauma, as seen on anterior rhinoscopy
Septal haematomas if left untreated can result in avascular necrosis of the septal cartilage, as the cartilage ordinarily gets its blood supply from the overlying perichondrium. This leaves the cartilage acutely susceptible to infection and abscess formation*.
Avascular necrosis over a longer period of time can also result in septal perforation or a “saddle nose” deformity due to weakened cartilage support of the nose (Fig. 3). As such, early recognition and intervention is essential, and should be assessed for in every patient presenting with nasal trauma.
*Nasal septal abscesses carry a risk of ascending cavernous sinus infection and the associated intracranial or ocular complications, as it is within the ‘danger zone’ of the face
Nasal Fracture
Nasal bone fractures account for nearly 50% of all facial fractures. However, the nose is usually too swollen initially to be effectively examined to determine a suitable management plan.
There is no role for plain film radiographs in the clinical diagnosis or management of isolated nasal injury; in cases where co-existing fractures are suspected, CT imaging is usually the preferred imaging modality.
Once septal haematoma has been ruled out by the initial assessment, patients with suspected nasal fractures can be seen semi-electively (usually within 7-10 days post-injury) in the ENT clinic, being assessed for:
- Nasal deformity– objective assessment for any bony or septal deviation including nasal step deformity, as well as the patient’s perception of the appearance of their nose
- Nasal obstruction – ask how the patient is symptomatically; air flow can be assessed by holding a metal tongue depressor below the nose and observing misting during nasal breathing

Figure 4 – Nasal deformity following a nasal fracture
If indicated, a Manipulation Under Anaesthesia (MUA) of the nasal bones can be performed, either under local anaesthetic (in the clinic) or general anaesthetic. This should take place within 14-21 days of the original injury.
If the aesthetic result is unsatisfactory, further definitive surgery can be performed. Rhinoplasty is concerned with changing the shape of the nasal bones, septoplasty is concerned with nasal septum alteration to improve nasal airflow.
Manipulation Under Anaesthesia of a Nasal Fracture
In order to reduce a nasal fracture under local anaesthetic, a regional nose block should be performed, typically using lidocaine with adrenaline.
When the nose is adequately anaesthetised, firm lateral digital pressure should be applied just below the area of deformity with the aim of straightening and aligning the nasal dorsum.
It is worth noting that correction of a dorsal hump is rarely achievable using this method.
Traumatic epistaxis
Epistaxis as a result of trauma is common*. In the majority of cases the bleeding will cease with simple measures, including applying firm pinching pressure onto the cartilaginous aspect of the nose.
Unless the injury is complicated by co-existing facial fractures, any epistaxis that does not resolve with these initial measures can be treated as per usual management steps (discussed here).
*Epistaxis from major trauma usually originates from the ethmoidal arteries (anterior primarily), therefore often are more likely to require operative intervention.
Complications
Whilst the majority of nasal trauma is uncomplicated such as obstructed nasal airflow, or minor deformity to the nose, complications can occur:
- CSF leak occurs following fracture through the cribiform plate (the roof of the nasal cavity), resulting in the leakage of CSF out via the nose; this may manifest clinically as persistent clear rhinorrhoea
- CSF can be confirmed by testing the fluid for high levels of beta-2 transferrin; in such cases, routine use of prophylactic antibiotics is not recommended and if the defect is small, a conservative approach can be adopted*
- Anosmia can also occur following nasal trauma; in the acute setting, this is typically due to the nasal passages being blocked with blood, however if post-traumatic anosmia persists, it is likely a result of damage to olfactory structures and unfortunately is unlikely to resolve.
*95% of cases will seal spontaneously within 2 weeks, however if CSF rhinorrhoea persists, surgical management may be required
Key Points
- In all nasal trauma, first consider any co-existing trauma that may require concurrent or prioritised treatment
- Be sure to check for a septal haematoma in all nasal trauma, even if there is a delay in presentation
- Patients with suspected nasal fractures can be seen semi-electively in an ENT clinic
- Most cases of CSF rhinorrhoea will resolve spontaneously and antibiotic prophylaxis is not required