This article is for educational purposes only. It should not be used as a template for consenting patients. The person obtaining consent should have clear knowledge of the procedure and the potential risks and complications. Always refer to your local or national guidelines, and the applicable and appropriate law in your jurisdiction governing patient consent.
Overview of Procedure
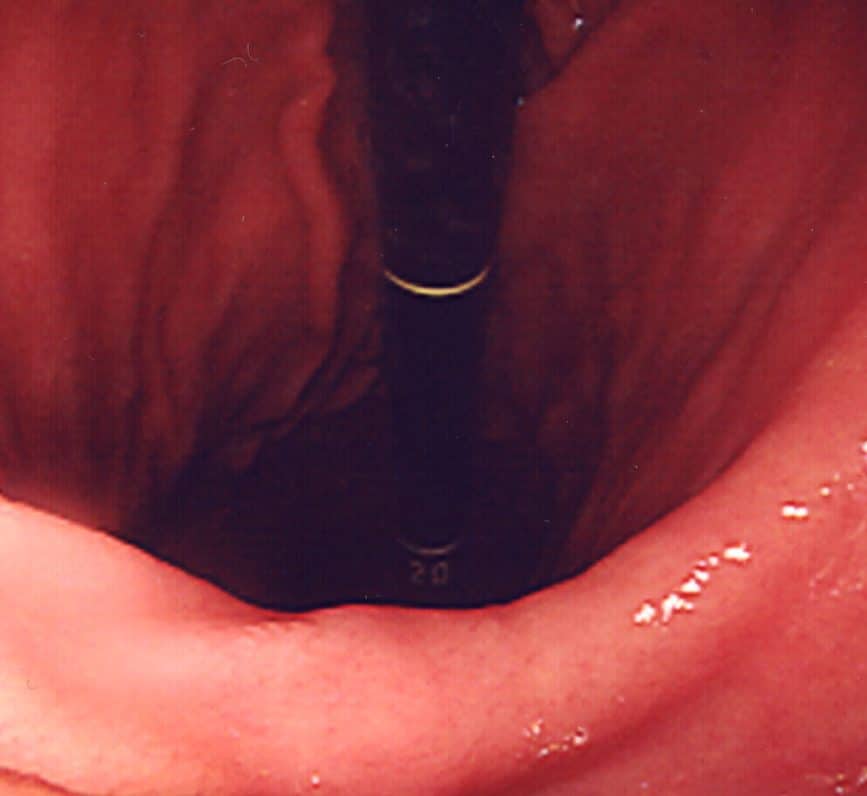
An oesophagogastroduodenoscopy (OGD) involves an inspection of the oesophagus, stomach, and proximal duodenum with a flexible endoscope.
This is often done with the aim of assessing the upper GI tract for a variety of symptoms, such as persistent dyspepsia, haematemesis, unexplained weight loss, and iron-deficiency anaemia. Biopsies can be taken if required, depending on the findings or indication.
Complications
Intra-Operative
| Complication | Description of Complication | Potential Ways to Reduce Risk |
| Haemorrhage | Damage to the oesophagus or stomach (or particularly any varices present) may cause significant bleeding, as well as from any biopsy sites | |
| Perforation | Although rare, this can occur (particularly if there is an upper GI cancer or pharyngeal pouch) | |
| Sedation risk | Sedatives, such as midazolam, are often used yet can depress the cardio-respiratory system | Always use monitoring and beware of using sedation in frail patients with co-existing cardio-respiratory disease or morbid obesity |
| Damage to teeth | Any loose teeth can potentially be dislodged during the procedure by the scope | Use a modified mouth guard for patients to allow the scope to pass by the teeth |
| Aspiration | Risk of gastric contents entering the lung during the procedure | Avoid heavy sedation and ensure prolonged fasting before the procedure |