Introduction
A liver abscess typically results from a bacterial infection spreading from the biliary or gastrointestinal tract, either via contiguous spread or seeding from the portal and hepatic veins.
Common causes include infective colitis, cholecystitis, cholangitis, diverticulitis, or appendicitis. Themost commonly isolated organisms are E. Coli, K. pneumoniae, and S. constellatus, although fungal causes may also be present in immunocompromised patients.
Clinical Features
Patients typically present with fever, rigors, and abdominal pain. Other symptoms include bloating, nausea, anorexia, weight loss, fatigue and jaundice.
On examination, patients will have right upper quadrant tenderness, although hepatomegaly is rarely present. If the abscess ruptures (a rare complication), then patients will present with peritonitis and features of septic shock.
Investigations
Blood tests will show a raised white cell count and liver function tests often are deranged, with a raised ALP in majority and possibly a raised ALT and bilirubin. All patients with suspected liver abscesses should also have peripheral blood cultures sent for microscopy.
Any fluid obtained from the liver abscess should be sent for fluid microscopy and culture. Echinococcal and amoebic serology should be checked for all abscess to exclude these rarer causes.
Ultrasound imaging can be used to confirm the diagnosis, demonstrating poor-defined lesions with hypo- and hyper-echoic areas, with potential gas bubbles and septations.
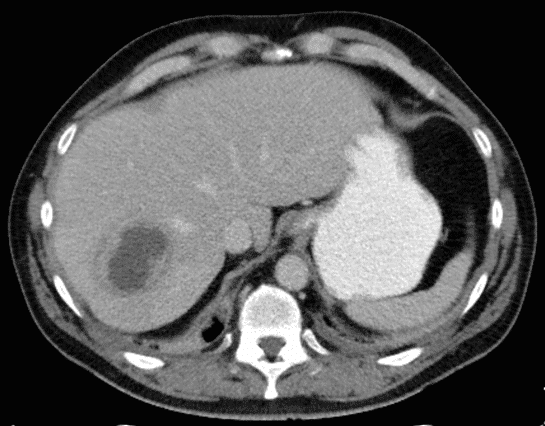
Further delineation can be achieved by CT imaging with contrast (Figure 1), useful for the diagnosis of the abscess, to plan definitive management, and identify any underlying pathology (e.g. biliary or bowel inflammation).
Management
Patients with a confirmed liver abscess should be started on intravenous antibiotics, initially empirically as per local guidelines, and then guided by sensitivities once available.
Large abscesses should be drained via image-guided aspiration of the abscess (with or without catheter drainage), either via ultrasound or CT-guidance, both for source control and identification of antimicrobial sensitivity.
There is no consensus on which size abscesses require drainage as most will respond to prolonged antibiotic treatment alone. Failure of antibiotic treatment, as defined by clinical course and interval imaging, is the most common trigger for radiological intervention.
Any underlying cause should also be addressed once the patient has been appropriately managed. Surgery is rarely indicated, usually only if the abscess has ruptured or refractory to antibiotic treatment.
Amoebic Abscess
An amoebic abscess is the most common extra-intestinal manifestation of amebiasis infection, caused by the organism Entamoeba histolytica.
The infection spreads via faeco-oral route, and once in the colon, the trophozoite invades the mucosa and spreads to the liver via the portal venous system.
It is estimated that 12% of the world’s population is infected with this organism, most commonly in developing regions such as South America, the Indian subcontinent, and Africa.
Clinical Features
Patients will present with vague symptoms of abdominal pain, nausea, fever or rigors, weight loss, and bloating. Cases should be suspected in particular for patients with a history of recent travel (<6 months) to an endemic region.
Patients may also report a prodrome of clinical features secondary to the intestinal involvement, including abdominal pain and diarrhoea.
Investigations
As with most abscesses, blood tests will show a raised white cell count and liver function tests often are deranged, with a raised ALP in majority and possibly a raised ALT and bilirubin. Serology will also be positive
Patients should also have peripheral blood and fluid cultures sent for microscopy. Blood and stool samples should also be sent to check for the presence of E. histolytica antibodies
Ultrasound imaging will reveal poor-defined lesions, which can be further characterised by CT imaging.
Management
Most patients can be treated with antibiotics alone, typically metronidazole or tinidazole as the antimicrobials of choice.
In large abscesses or those which do not respond well to antibiotic therapy, surgical drainage may be required. A luminal agent, such as paromomycin, can also be prescribed to eradicate amoebiasis in the colon.
Key Points
- Liver abscess should be considered in all patients presenting with pyrexia of unknown origin associated with associated abdominal pain or bloating
- For all cases of liver abscess, it is important to investigate and treat any underlying cause
- Liver abscesses can often be treated with image-guided drainage, however amoebic abscesses can be managed through antibiotic therapy alone