Introduction
Few injuries are as potentially catastrophic as spinal fractures. These fractures range from the wedge fracture to the life-changing fracture-dislocation with an associated spinal cord injury.
Spinal fractures tend to occur at zones of mechanical transition. The thoracolumbar junction (T11–L2) is the most commonly fractured region, with 40-60% of all spinal fractures occurring at these levels.
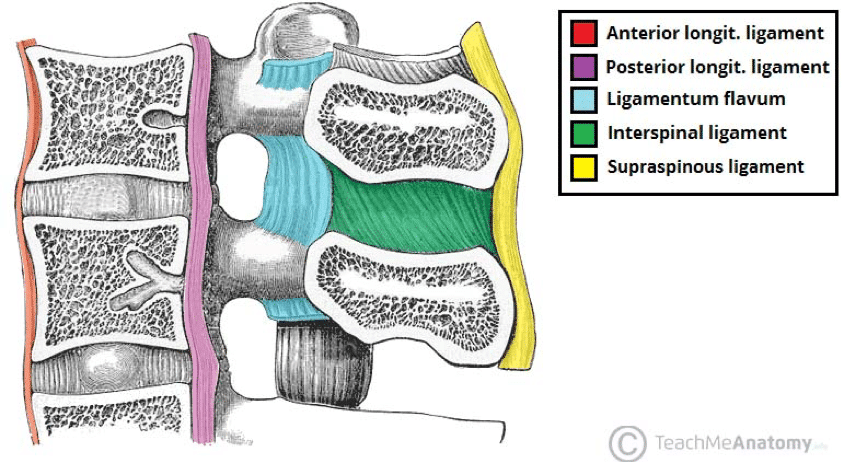
The spine may be thought of as consisting of three columns (Fig. 1), which are important when assessing the stability of a fracture:
- Anterior column – anterior longitudinal ligament and the anterior half of the vertebral body and disc
- Middle column – posterior half of the vertebral body and disc, and posterior longitudinal ligament
- Posterior column – comprised of the posterior elements (the posterior ligamentous complex, including the facet joint capsule, ligamentum flavum, and interspinous and supraspinous ligaments) and the intervening vertebral arches
Classification
Thoracolumbar fractures can be classified based on their morphology according to the AO classification:
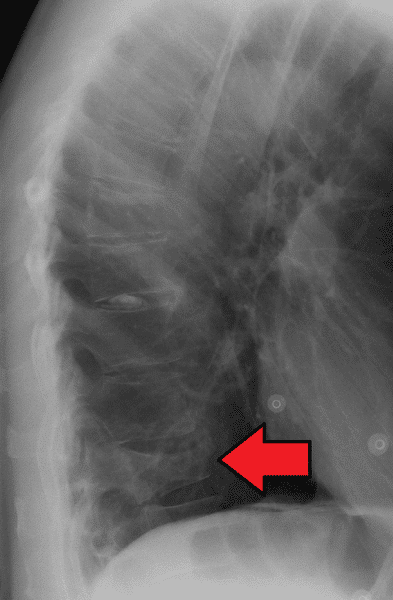
- Type A – compression injuries (Fig. 2 & 3)
- Type B – distraction injuries
- Type C – translation injuries
Burst Fracture
A burst fracture occurs when there is a substantial compressive force acting through the anterior and middle column of the vertebrae, resulting in retropulsion of bone into the spinal canal. This can result in potential spinal cord injury. These fractures can involve one end plate (incomplete burst) or both endplates (complete burst).
Chance Fracture
Chance fractures are vertebral fractures that result from excessive flexion of the spine and involve all three spinal columns. These are unstable injuries and will often need surgical intervention to stabilise. They classically occur following head-on road traffic accidents in which the affected person is wearing only a lap belt, therefore are commonly associated with concurrent abdominal injuries.
Clinical Features
A sizeable proportion of thoracolumbar fractures occur in patients with underlying osteoporosis, often the fractures only occurring from low impact injuries. Among younger patients, thoracolumbar fractures are usually the result of high-energy trauma.
Patients will most commonly present with back pain, but this is not always the case, especially if there are concurrent (i.e. distracting) injuries or if the fracture was sustained insidiously.
There may be varying degrees of neurological involvement present, depending on the level of spinal cord involvement (further discussed here). As such, a thorough neurological examination is required for patients with a suspected thoracolumbar vertebral fracture.
Differential Diagnosis
There are a wide range of causes for back pain following an injury, which can include disc prolapse, degenerative diseases of the spine, malignancy (either primary or metastatic), or infection (including osteomyelitis).
Investigations
Current NICE guidelines state that the following imaging should be completed:
- Perform a plain film radiograph* as the first‑line investigation for those with suspected spinal column injury without abnormal neurological signs or symptoms
- Perform a CT scan if the radiograph is abnormal or there are clinical signs or symptoms suggestive of a spinal column injury
- If a new spinal column fracture is confirmed, image the rest of the spinal column
Whilst CT imaging has become the mainstay for cervical fracture diagnosis, MRI imaging is also useful to assess for concurrent injury of soft tissue structures of the spine, such as the intervertebral discs, spinal cord, nerve roots and posterior ligaments.
Pathological causes should be suspected, especially in younger cases or in those following low-impact injuries, and further work-up, including a serum calcium and myeloma screen, may be warranted.
*For plain film radiographs, 2 separate views are required, with the AP looking at the alignment of the spinous processes and for any widening or displacement of the pedicles, whilst the lateral view assesses overall alignment, vertebral body height, and spacing between the posterior bony elements
Management
Patients with a suspected thoracolumbar fracture must be managed as per ATLS guidance, including appropriate immobilisation.
Restricting movement of the spine is recommended to prevent damage to the spinal cord. Movement at the level of an unstable fracture can cause further neurological deficit, and so patients suspected of having a spinal fracture should be handled with the minimum amount of force and movement applied to the spine
Non-operative management is often indicated in the more stable thoracolumbar fractures. Options include extension bracing and lumbar corsets that aim to resist progressive kyphosis and support the spine, also being used to provide comfort and assist mobility in stable thoracolumbar injuries.
Adequate analgesia and physiotherapy is essential as part of the rehabilitation.
Surgical Intervention
The Thoraco-Lumbar Injury Classification and Severity (TLICS) scoring system (Table 1) can be used to quantify the likelihood of instability and the requirement for surgery*.
Operative management usually involves decompression and instrumented spinal fusion. Stabilisation is most commonly performed via a posterior approach with the patient lying prone, and fixation is achieved using pedicle screws and rods.
*Whilst not prescriptive, injuries that score 5 or more are considered unstable and are usually treated surgically and those that score 3 or less are usually considered stable and treated conservatively.
|
Parameter |
Points |
| Morphology | Wedge compression fracture = 1 point
Burst fracture = 2 points Translation / rotation fracture = 3 points Distraction fracture = 4 points |
| Integrity of Posterior Ligamentous Complex | Intact = 0 points
Suspected or indeterminate = 2 points Injured = 3 points |
| Neurological Status | Intact = 0 points
Nerve root = 2 points Cord or conus medullaris (incomplete) = 3 points Cord or conus medullaris (complete) = 2 points Cauda equina = 3 points |
Table 1 – The Thoraco-Lumbar Injury Classification and Severity Scoring System
Key Points
- The thoracolumbar junction (T11–L2) is the most commonly fractured region
- A CT scan should be performed in suspected thoracolumbar fractures with clinical features suggestive of a spinal cord injury
- Non-operative management is often indicated in the more stable thoracolumbar fractures.