The normal range for intracranial pressure (ICP) is 5 – 15mmHg. The average intracranial volume is 1700ml (composed of the brain 1400ml + CSF 150ml + blood 150ml), with Cerebrospinal Fluid (CSF) production around 500 – 600ml per day.
The skull is a rigid compartment, and the Monro-Kellie doctrine describes a pressure-volume relationship, a dynamic equilibrium among components within the rigid skull compartment:
VIntracranial = VBrain + VCSF + VBlood
In order to protect the brain, the blood and CSF volume can be comprised as the primary protection. However, this mechanism can be overcome with large increases to these volumes.
This article discusses the importance of ICP monitoring and how it can be performed.
Cerebral Perfusion Pressure
Cerebral perfusion pressure (CPP) drives oxygenation and metabolite transfer to cerebral tissues.
The brain can autoregulate blood flow, through cerebral vessel constriction or dilatation, in order to ensure constant flow isolated from fluctuations in systemic blood pressure*; the Cerebral Perfusion Pressure is calculated by Mean Arterial Pressure minus Intracranial Pressure.
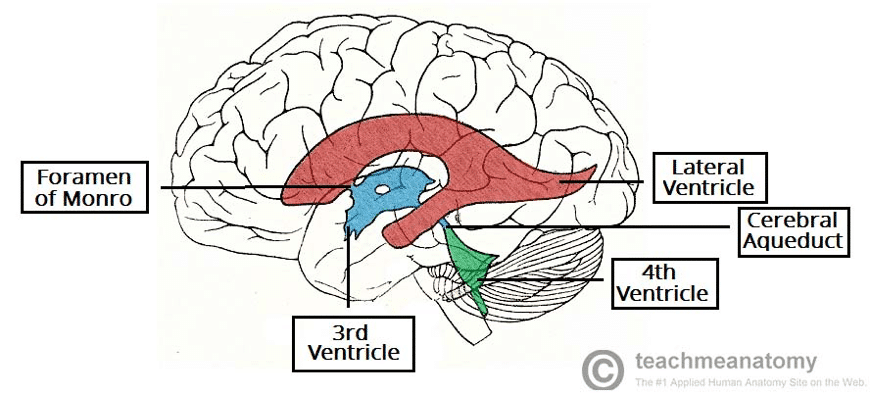
CSF is produced by ependymal cells within the choroid plexus and circulates within the ventricular system, being reabsorbed via arachnoid granulations. There is normally an equilibrium between CSF production and absorption, however when this relationship is disrupted, a raised ICP can occur
*This is the mechanism that is often lost due to head trauma, leading to cerebral ischaemia and neuronal death (secondary brain injury)
Clinical Features
The clinical features of raised ICP will progress from initial mild non-specific symptoms to late significant symptoms.
Early onset symptoms include morning headache (worse upon coughing, exertion or moving head), vomiting (with no associated nausea), and lethargy or altered mental status.
On examination, there may be ocular palsies, papilloedema, or pupil irregularities, including unilateral dilation or pupillary light defects
Late features include persistent vomiting, Cushing’s triad*, ophthalmoplegia, and eventual coma and death.
*Cushing’s Triad is composed of irregular respiration, bradycardia, and systolic hypertension (with wide pulse pressure)
Indications for ICP Monitoring
Whilst ICP monitoring is most commonly used for the management of severe head trauma, its use also extends to CSF circulatory disorders, and can be either diagnostic or therapeutic (by removing CSF to reduce pressures).
Current indications for ICP monitoring include traumatic brain injury (TBI), hydrocephalus or conditions at high risk of developing hydrocephalus (e.g. space-occupying lesions or subarachnoid haemorrhage), idiopathic intracranial hypertension, or Reye’s syndrome
Contra-indications to ICP monitoring include coagulopathies or anti-coagulation medication, scalp infections, or brain abscess.
The main complications following ICP monitor insertion are infection (meningitis, ventriculitis, wound infection), intracranial haemorrhage, device malfunction or difficulty with placement, and ventricular collapse (potentially leading to tentorial herniation).
Types of ICP Monitors
There two basic ICP monitor types are via ICP data only (commonly known as ‘bolts’) or ICP data plus CSF drainage. The three main types of ICP monitor are the External Ventricular Drain (EVD), the Subarachnoid Bolt, and the Epidural bolt (Fig. 2).
These probes can often also be used to measure other physiological parameters, including temperature, lactate, and pH.
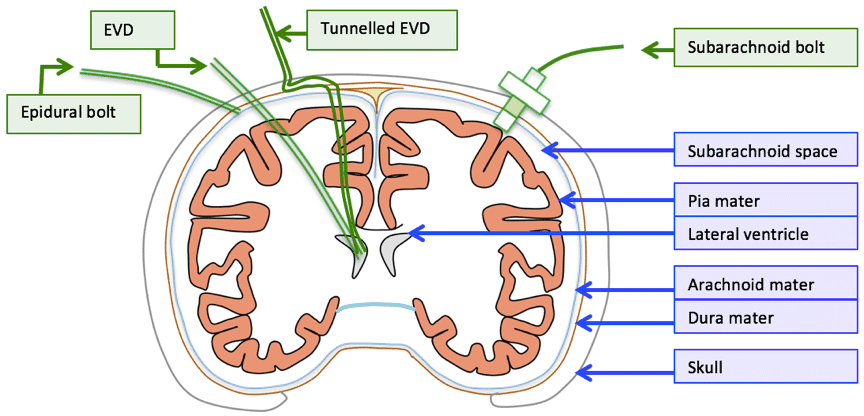
Figure 2 – Schematic representing the anatomical insertion site for ICP monitoring
Subarachnoid Bolt
The subarachnoid bolt is a small and unobtrusive device, allowing for a good waveform resolution of ICP. It is relatively easy to install and is less invasive than EVD.
However, it does come with several limitations, including lack of therapeutic uses, unable to be recalibrated following installation, and the transducer tip becoming obstructed if it comes into contact with brain parenchyma, as well as a higher infection risk and lack of discrimination of infratentorial pressures.
Epidural bolt
An epidural bolt also has the limitation of a lack of therapeutic use. It also has more pronounced signal attenuation so often will underestimate the ICP. However, it does have a decreased infection risk, which confers advantage over the subarachnoid bolt.
External Ventricular Drain
The External Ventricular Drain (EVD), also termed fluid-filled transduced ventriculostomy, is the gold standard intervention for raised ICP*
Its main benefits include additional uses for therapeutic aspiration of CSF, rarely will occlude, and inexpensive, albeit difficult to install. Its limitations include infection (ventriculitis) and potential for damage to the underlying brain parenchyma.
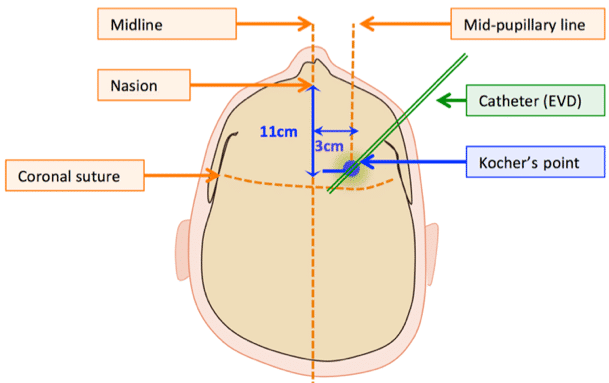
They are most commonly inserted into Kocher’s point, however alternative points for EVD insertion include Keen’s point, Frazier’s point, and Dandy’s point
*Global CSF pressure is better reflected by ventricular pressure as opposed to subdural, extradural, or subarachnoid pressure
The External Ventricular Drain Procedure
An incision should be made at Kocher’s point (Fig. 3) and a burr hole made at this site. Open the dura and insert a catheter into the anterior horn of lateral ventricle; CSF will appear via catheter.
Tunnel away from burr hole site posterolaterally and suture in place. Confirm drain placement using CT imaging.
Attach the catheter to non-pressurised tubing filled with saline solution and connected to non-flush strain-gauge transducer (this will measure the pressure transmitted from CSF in the ventricles). Level the transducer to zero.
ICP Monitoring Waveforms
The waveforms produced from the ICP monitoring can be used to infer the underlying pathology present. The wave forms produced are summarised in Table 1.
| Wave phase | Wave name | Represents |
| P1 | Percussion | Arterial pulsation |
| P2 | Tidal | Intracranial compliance |
| P3 | Dicrotic | Aortic valve closure |
Table 1 – Waveforms characteristics from ICP monitoring
The height order of the wave phases on monitoring should be P1 > P2 > P3. If P2 is highest, this indicates potential raised ICP (Fig. 4).
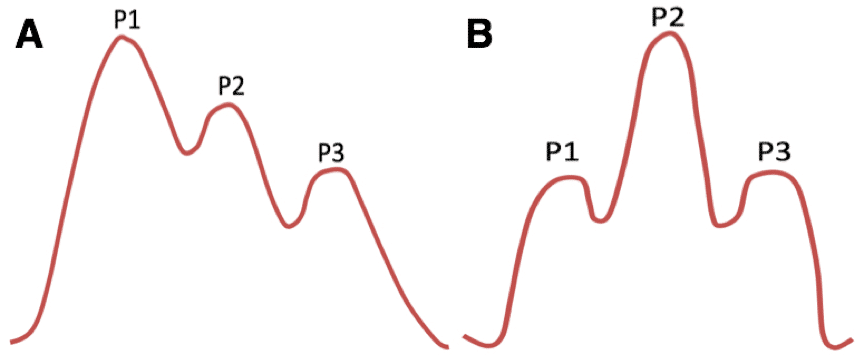
Figure 4 – (A) showing normal ICP waveforms (B) showing ICP waveforms in keeping with raised ICP
Key Points
- Pressures above 20mmHg usually represent the threshold to treat raised ICP.
- Most common ICP monitoring indication is severe TBI.
- The three main interventions for ICP monitoring are External Ventricular Drain, subarachnoid bolt, and epidural bolt.
- Monitors are usually inserted at Kocher’s point.
- ICP monitoring must be overseen by trained professionals, regularly checking calibration and the tubing.