This article is for educational purposes only. It should not be used as a template for consenting patients. The person obtaining consent should have clear knowledge of the procedure and the potential risks and complications. Always refer to your local or national guidelines, and the applicable and appropriate law in your jurisdiction governing patient consent.
Overview of Procedure
Retrograde ureteric stent insertion is the passage of a stent to relieve a ureteric obstruction, most commonly from from stones or urethral strictures.
Via rigid cystoscopy, the stent is passed into the ureter (via the urethra and bladder, i.e. retrograde) under X-ray or ultrasound guidance using a guidewire.
Both ends of the stent are subsequently coiled to prevent displacement. The stent may be removed after several days, weeks, or months after insertion depending on the clinical indication.
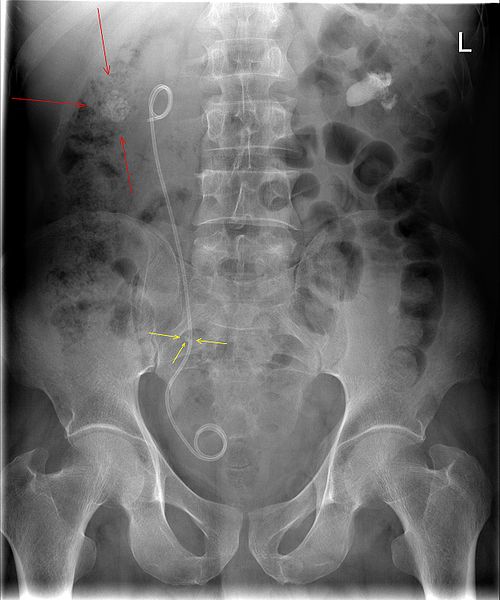
Figure 1 – A plain film abdominal radiograph showing a JJ ureteric stent in-situ, with associated renal (red arrow) and ureteric (yellow arrow) stones
Complications
Intraoperative
| Complication | Description of Complication | Potential Ways to Reduce Risk |
| Haemorrhage | Damage to surrounding blood vessels or intraluminal damage to the urinary tract | Careful and meticulous handling of the instruments to avoid damage |
| Damage to surrounding structures | Damage can occur to the urethra, bladder, or ureters during the procedure | |
| Allergic reaction | Local anaesthetic toxicity or reaction to instruments used | |
| Anaesthetic Risk | Includes damage to the teeth, throat and larynx, reaction to medications, nausea and vomiting, cardiovascular and respiratory complications | Forms a part of the anaesthetist assessment before the operation |
Early
| Complication | Description of Complication | Potential Ways to Reduce Risk |
| Pain | Suprapubic or flank pain due to bladder irritation from stent placement | |
| Infection | Infection can be introduced by the instrumentation | Maintain an aseptic technique throughout the procedure |
| Bleeding | Damage to intraluminal surfaces of the urinary tract, resulting in haematuria | |
| Stent displacement | Migration of the stent from its original position | |
| Technical failure | Difficult anatomy leading to abandoning of procedure and may result in further operation | |
| Blood clots | DVTs and PEs are a possibility in any operation, yet often the procedure is often short so the risk is low | The patient will be given anti-embolism stocking and low molecular weight heparin peri-operatively to minimise this risk as deemed appropriate |
Late
| Complication | Description of Complication | Potential Ways to Reduce Risk |
| Stent blockage or encrustation | Results from bacterial colonisation of the stent and subsequent crystal deposition | Regular stent changes |
| Reintervention | Blocking of the stent may require reintervention |
