Introduction
Neck lumps are a common presentation in the general population and have a number of possible causes. As such, comprehensive history and examination is required, before considering appropriate investigations.
In this article, we shall discuss the differential diagnoses, investigations, and management of a patient presenting with a neck lump.
Clinical Features
The first step in the assessment of a patient with a neck lump is to take a detailed history and perform a comprehensive examination.
Key parts of the history:
- Duration of onset
- Any recent change in size, number of neck lumps
- Associated symptoms (especially red flag symptoms, discussed below)
- Relevant past medical history – smoking status, alcohol intake, previous head and neck cancers, and known radiation exposure (e.g. previous radiotherapy)
Key parts of the examination:
Any lump in the neck can be metastatic lymphadenopathy secondary to malignancy in the nasopharynx, oropharynx, hypopharynx and the oral cavity. Therefore, it is essential to examine all of these areas to rule out any sinister causes.
- Neck – described here
- Oral cavity – described here
- Ear- described here
- Cranial nerve examination – described here
Red Flags for a Neck Lump
In the context of a neck lump, the “red flag” features raise the suspicion of an underlying head and neck malignancy.
- Hard, painful and fixed lump
- Associated otalgia, dysphagia, stridor, or hoarse voice
- Unilateral nasal symptoms such as epistaxis, discharge, or congestion
- Unexplained weight loss, night sweats, or fever or rigors
- Cranial nerve palsies
In children, red flag symptoms also include the presence of a supraclavicular mass, lumps larger than 2cm, and a previous history of malignancy.
Differential Diagnoses
The possible causes of a neck lump can be formulated using a ‘surgical sieve’:
- Infective
- Reactive lymphadenopathy – increase in size of the cervical lymph nodes in response to infection
- Sialadenitis
- Neoplastic
- Lymphoma – a haematological malignancy that commonly causes lymphadenopathy
- Head and Neck Cancer or Salivary Gland Tumour
- Metastatic disease spread
- Skin lump, ranging from benign (e.g. lipoma) to malignant (skin cancer)
- Vascular
- Carotid body tumour (see below)
- Inflammatory
- Sarcoidosis
- Traumatic
- Autoimmune
- Thyroid disease, such as Graves’ disease
- Congenital
- Cystic hygroma (see below)
- Thyroglossal cyst (see below)
- Branchial cyst (see below)
- Dermoid cyst – a cystic type teratoma, form along the lines of embryological fusion, can present as midline painless lumps, more common in children and young adults
Investigation
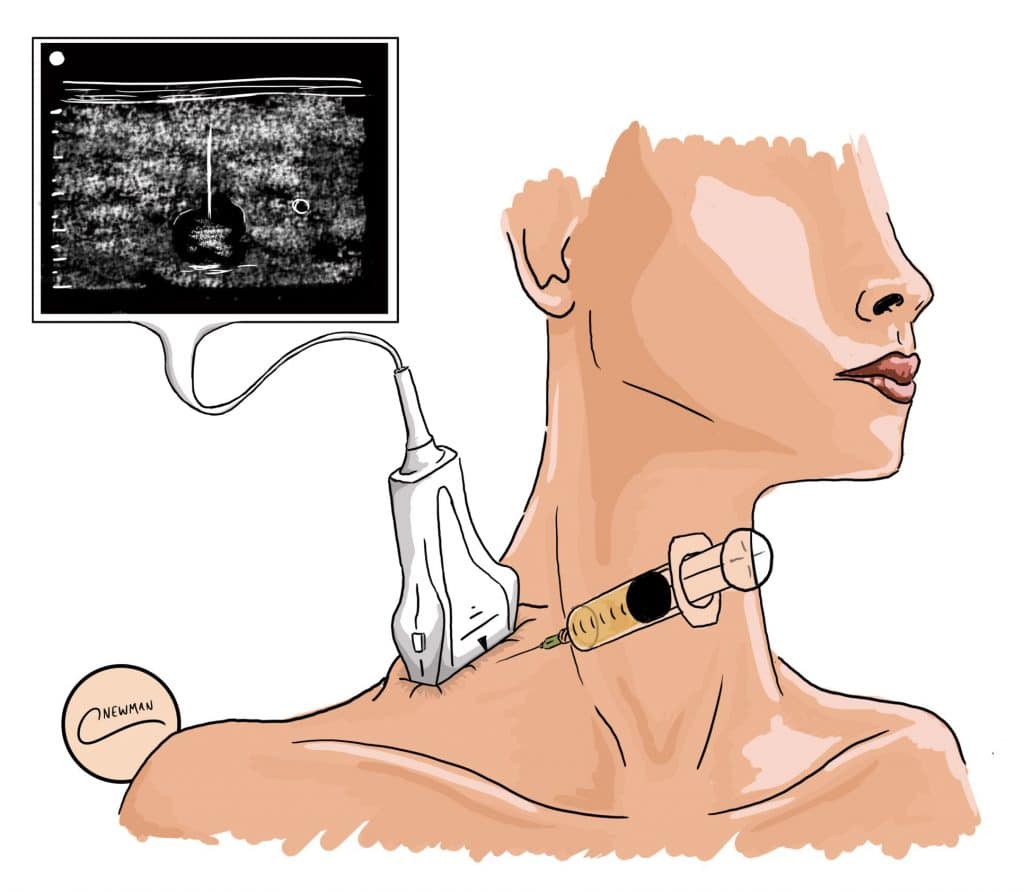
The first-line investigation for a suspicious neck lump is ultrasound +/- fine needle aspiration (FNA).
Ultrasound provides characterisation of lymph nodes, salivary glands, vascular structures, and thyroid nodules. Indeed, ultrasound findings alone can be sufficient to make a diagnosis of certain neck lumps.
If there are suspicious features on imaging, an ultrasound-guided FNA (Fig. 2) should be performed (unless lymphoma is suspected, then a core biopsy or an open excision biopsy is preferable in this case).
If further imaging is needed to assess a neck lump, CT or MRI imaging may be carried out. CT provides visualisation of bony anatomy, whilst MRI provides soft tissue detail and delineation of abnormalities in the oral cavity or oropharynx.
Current guidelines advise both CT and MRI also aid in the management of head and neck cancer, including staging disease, detecting metastases, and radiotherapy planning.
Cystic Hygroma
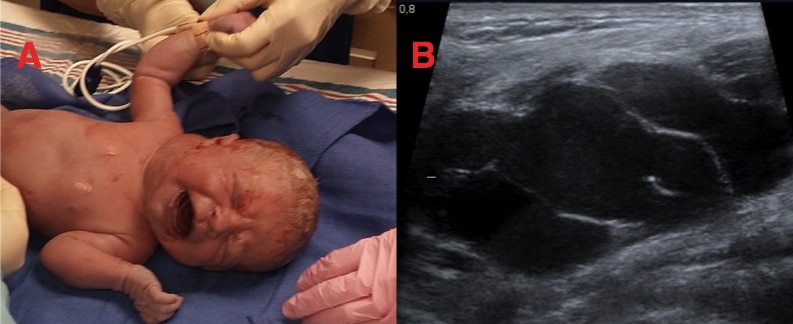
A cystic hygroma (also known as a cystic lymphangioma) is a benign fluid-filled sac caused by a malformation of the lymphatic system. They can be found anywhere on the body, but classically presents in the axilla or posterior triangle of the neck.
Cystic hygromas are typically noticed and diagnosed before aged two years* (Fig. 3A), presenting as soft painless fluctuant masses that transilluminate. They can be associated with congenital conditions (e.g. Turners syndrome) and can grow large enough to cause airway obstruction or dysphagia.
However, not all cystic hygromas require treatment, unless symptomatic. Treatment options include surgical excision (associated with low risk of recurrence) or lymphatic sclerotherapy (injection of sclerosing agents into the cyst).
*In some cases, a cystic hygroma is diagnosed antenatally and if it is likely to cause airway compromise at birth, an Ex Utero Intra-Partum Treatment (EXIT) procedure can be performed
Carotid Body Tumours
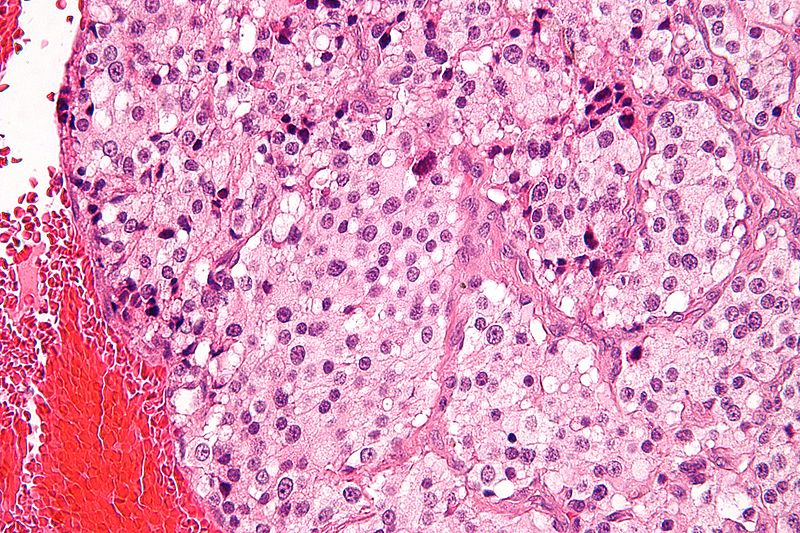
Carotid body tumours (also known as a carotid paragangliomas) are benign neuroendocrine tumours that arise from the paraganglion cells of the carotid body. The carotid body is made up of a cluster of neuroendocrine cells, whereby sporadic (or hereditary) mutations lead to the formation of paragangliomas (Fig. 4).
A carotid body tumour will present as a pulsatile painless neck lump, often with a bruit present on auscultation*. Carotid paragangliomas are slow growing, but can become large enough to compress surrounding cranial nerves, leading to palsies. Rarely, patients can present in cardiac arrhythmia if the carotid sinus is stimulated by compression from the tumour.
Carotid body tumours can be managed conservatively with active monitoring via serial imaging, or require surgical excision in a specialised unit with both ENT and vascular input. Radiotherapy may be an option for tumours that are unresectable, to limit tumour growth.
*Classically carotid body tumours can be moved from side to side but not up and down, due to their location in the carotid sheath, termed Fontaine’s sign
Thyroglossal Cyst
A thyroglossal cyst is a congenital fluid filled sac, commonly presenting in younger patients (typically <20yrs) and have equal incidence between men and women.
Embryology of Thyroglossal Cysts
During embryonic development, the thyroid gland originates from the base of the tongue (foramen caecum), migrating down to its final position in the neck and connecting back to the tongue via the thyroglossal duct.
In normal development, this duct will obliterate, however thyroglossal cysts occur when portions of this duct remain patent, creating cavities that may fill with fluid and being prone to infection.
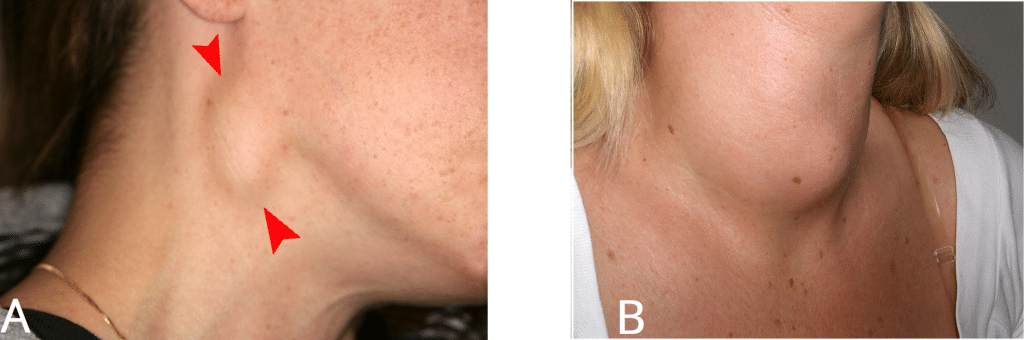
Thyroglossal cysts present as a palpable painless midline mass* (Fig. 5A) that move up with swallowing and protrusion of the tongue. When infected, they can increase in size and become painful.
Standard treatment is surgical intervention, with the modified Sistrunk procedure being the most widely used. The central body of the hyoid bone is removed to allow complete removal of the entire thyroglossal tract. There is a high chance of recurrence if the medial portion of the hyoid bone is not removed.
It is essential that these patients have an ultrasound scan of the neck to identify the thyroid gland pre-operatively, as the only functioning thyroid tissue may be attached to the cyst and risks getting excised during the procedure.
*In rare cases (~1%), patients may develop thyroglossal duct cyst carcinoma that often arises from ectopic thyroid tissue in the cyst (the most common histology is papillary carcinoma)
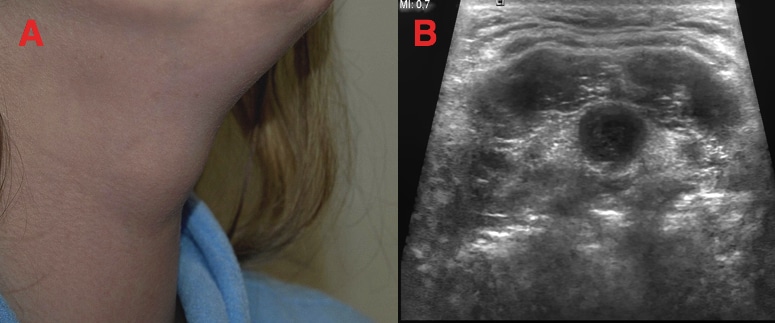
Figure 5 – (A) A simple thyroglossal cyst (B) Ultrasound findings of a thyroglossal cyst
Branchial Cyst
Branchial cysts are congenital masses which arise in the lateral aspect of the neck, typically anterior to the sternocleidomastoid (SCM).
During the fourth week of development, branchial clefts form ridges known as branchial arches, involved in the formation of a number of structures in the head and neck. Incomplete obliteration of these clefts will result in the formation of branchial cysts.
They present as palpable masses anterior to SCM, typically unilateral (Fig. 6). When infected, they can increase in size and become painful. Larger branchial cysts can result in dysphagia, dysphonia, and difficulty breathing.
Surgical excision is the definitive treatment. Sclerotherapy can be offered as an alternative to surgery in certain cases, involving injection of a sclerosing agent under ultrasound guidance.
Care needs to be taken when managing these patients as a common differential diagnosis is a cystic metastasis from a squamous cell carcinoma of the head and neck region (especially in the adult population). As such, an ultrasound-guided FNA is an important investigation prior to arranging for excision of the mass.

Figure 6 – A patient with large right branchial cyst, prior to excision
Key Points
- Neck lumps are a common presentation in the general population and have a wide range of potential differential diagnoses
- Investigation of a neck lump, following history and examination, if suspicious, will require ultrasound +/- fine needle aspiration
- If lymphoma is suspected, a core biopsy or an open excision lymph node biopsy will be preferred over fine needle aspiration to obtain histological diagnosis
- CT or MRI scanning may be carried out for further assessment once an initial diagnosis is made, especially if there are concerns of head and neck malignancy