Introduction
Supracondylar humeral fractures are a common paediatric elbow injury, but are almost never seen in adults.
The peak age of incidence is 5-7 years. The most common mechanism of injury is falling on an outstretched hand with the elbow in extension (a small percentage occur from landing directly onto a flexed elbow).
Due to the close proximity of surrounding neurovascular structures, injury is common and a careful thorough assessment is essential.
Clinical Features
Patients typically present following a recent fall or direct trauma, resulting in sudden-onset severe pain and reluctance to move the affected arm.
On examination, there may be signs of gross deformity, swelling, limited range of elbow movement (secondary to pain), and ecchymosis of the anterior cubital fossa. Ensure to look closely for evidence of an open injury.
It is essential to carefully examine the median nerve, the anterior interosseous nerve (the deep motor branch of the median nerve), the radial nerve, and the ulnar nerve.
Check the hand for features of vascular compromise, such as a cool temperature, pallor, delayed capillary refill time, or absent pulses. Urgent orthopaedic review is required for all supracondylar fractures, especially those with neurovascular compromise or evidence of an open fracture.
Differential Diagnosis
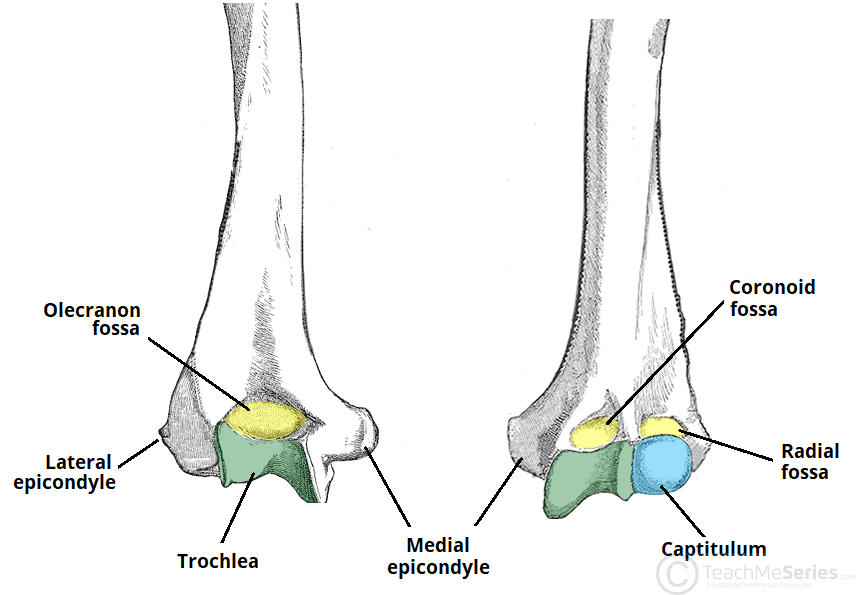
Distal humeral fractures and olecranon fractures are important fractures to exclude, as management of these can vary significantly. Other differentials include soft tissue injury or a subluxation of the radial head.
Investigations
The mainstay of investigation for suspected supracondylar fractures is via plain film radiographs in both antero-posterior (AP) and lateral views of the elbow.
Subtle signs on plain film radiograph for a supracondylar fracture include:
- Posterior fat pad sign (lucency visible on the lateral view)
- Displacement of the anterior humeral line (in children >5yrs, this should intersect the middle third of the capitellum)
CT imaging may be useful for comminuted fractures or where intra-articular extension is suspected, which aides with surgical planning.
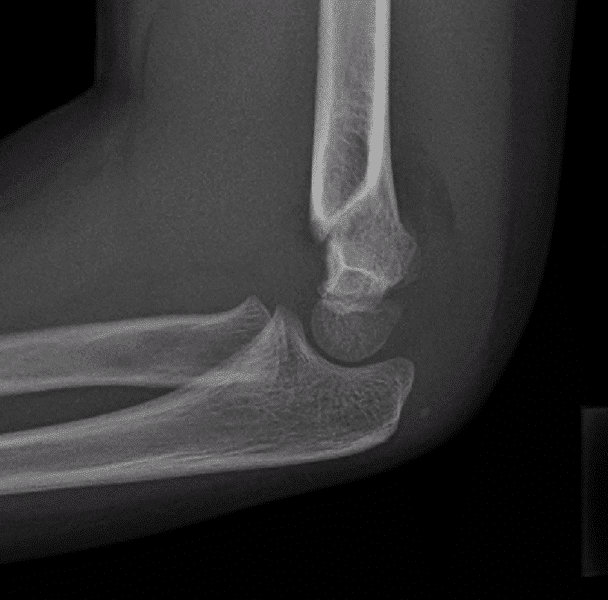
Figure 2 – Plain film radiograph of a supracondylar fracture in lateral view
Gartland Classification
The Gartland classification system of supracondylar fractures is a system commonly used in clinical practice, also aiding in management planning:
- Type I – Undisplaced
- Type II – Displaced with an intact posterior cortex
- Type III – Displaced in two or three planes
- Type IV – Displaced with complete periosteal disruption*
*Not part of the original Gartland Classification and can only be diagnosed intra-operatively
Management
Patients with supracondylar fractures with associated neurovascular compromise on presentation need immediate closed reduction. In children, this will invariably require this to be performed in theatre; the reduction is then secured with K-wire fixation (which can be removed in clinic after 3-4 weeks).
Conservative management can be trialled with type I fractures or minimally displaced Type II fractures, which can be managed in an above elbow cast in 90 degrees flexion.
Surgical Management
Type II, Type III, and Type IV supracondylar fractures will nearly always require a closed reduction and percutaneous K-wire fixation.
Open fractures warrant open reduction with percutaneous pinning. Any cases which fail closed reduction will also require open intervention.
Any ongoing vascular compromise, despite adequate reduction, may need discussion with vascular surgeons for potential vascular exploration.
Complications
Nerve palsies are common with supracondylar fractures, with neuropraxia rates around 10%; however, this rarely results in permanent damage. The anterior interosseous nerve is most commonly affected by the initial injury, however ulnar nerve palsy is the most common post-operative complication. The ulnar nerve is at risk during insertion of the medial K-wire.
Malunion is an important complication to assess for following a supracondylar fracture, more common in those fractures managed suboptimally. In some cases, patients may even develop a cubitus varus deformity (often termed “gunstock deformity”), whereby the extended forearm deviates towards the midline.
A Volkmann’s contracture can occur following vascular compromise with a supracondylar fracture. Ischaemia and subsequent necrosis of the flexor muscles of the forearm, eventually begins to fibrose and form a contracture; this results in the wrist and hand to be held in permanent flexion, as a claw-like deformity.
Key Points
- Supracondylar humeral fractures are a common paediatric elbow injury
- Patients typically present following a recent fall or direct trauma, resulting in sudden-onset severe pain
- The anterior interosseous nerve is most at risk of injury following supracondylar fractures
- Plain film radiographs form the mainstay of investigation
- Most cases will need a closed reduction and percutaneous K-wire fixation