Introduction
Vertigo is a specific symptom of hallucination of movement or spinning of the environment, often resulting in issues with balance.
Whilst aetiology varies, all causes of vertigo produce a conflict between the vestibular input and other sensory inputs of balance (i.e. proprioception and vision), resulting in the sensation of vertigo.
The causes of which can be divided into central or otological:
- Central causes of vertigo include multiple sclerosis, posterior stroke, migraine, or intracranial space occupying lesion
- Otological causes of vertigo include Benign Positional Paroxysmal Vertigo, Meniere’s Disease, and Vestibular Neuronitis
Balance disorders can be multifactorial and have a wide range of causes outside of disorders of the vestibular system or brain. It is important to consider alternative medical issues, such as circulatory/cardiac disease and metabolic issues. Indeed, in the acute setting, the most critical diagnosis to exclude is a posterior circulation stroke.
Benign Positional Paroxysmal Vertigo
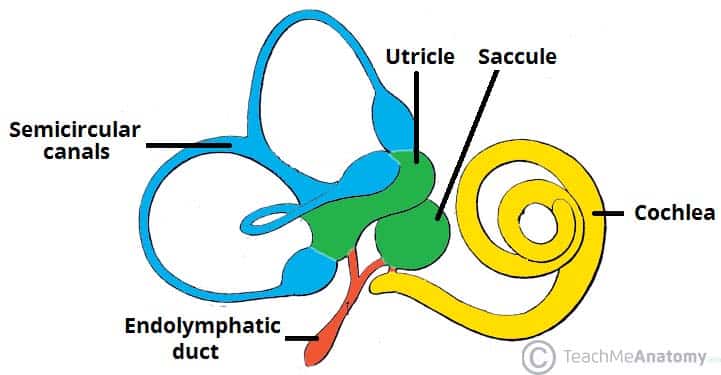
Benign Positional Paroxysmal Vertigo (BPPV) is caused by the presence of canaliths in the semi-circular canal instead of the utricle (Fig. 2).
Once in the canal, movement of the patient’s head will result movement of these crystals that cause an abnormal movement of endolymph, resulting in vertigo. Risk factors for BPPV include head injury, previous history of labyrinthitis, and older patients. That said, in most patients it is unprovoked.
Clinical Features
In BPPV, vertigo attacks last seconds and result from the same head movement causing the onset of symptoms every time. Accompanying symptoms typically include nausea or vomiting. A classical history is of vertigo when turning the head, e.g. movement of the head on the pillow in the morning.
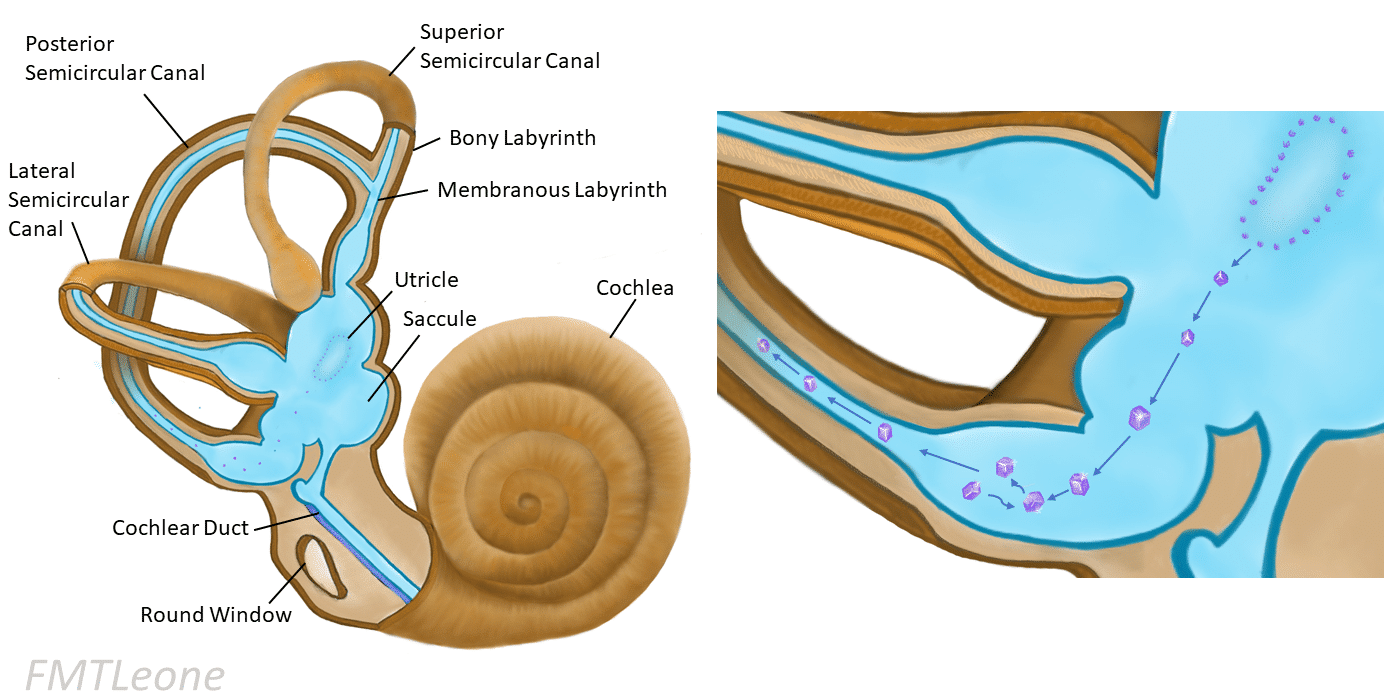
Figure 2 – Formation of crystals and their migration into the semi-circular canals in BPPV
Management
The diagnostic examination for BPPV is the Dix-Hallpike manoeuvre, with a positive test invoking the symptoms and nystagmus* will be present. The nystagmus will typically fatigue in less than a minute.
Once the condition is diagnosed, specific manoeuvres can be employed to remove the crystals from the canal and resolve the symptoms. A common manoeuvre is Epley’s Manoeuvre, performed if the canalith are in the posterior canal.
Patients post-Epley’s manoeuvre are advised not to drive, to keep sleep upright, not to bend down or look upwards for 48 hours. Resolution is not always complete, with some patients requiring repeated Epley’s as symptoms persist, and BPPV can also recur.
Patients can also be advised to perform Brandt-Daroff exercises, positions they can practice at home that are beneficial in reducing symptom intensity.
*Most commonly crystals form in the posterior canal, resulting in a rotatory nystagmus to be present; if in the horizontal canal then result in a horizontal nystagmus.
Meniere’s Disease
Meniere’s Disease is a disorder comprised with a triad of symptoms including vertigo, hearing loss, and tinnitus. Current theories in its pathophysiology suggest the symptoms result from an increase in endolymphatic pressure.
Caused by dysfunctioning sodium channels, an osmotic gradient is subsequently set up that draws fluid into the endolymph, increasing the endolymphatic pressure to cause symptoms.
Clinical Features
Meniere’s disease presents with attacks comprised of a triad of severe paroxysmal vertigo, sensorineural hearing loss, and tinnitus.
Symptoms are predominantly unilateral, lasting for minutes to hours, and usually resolve within 24 hours. During remission between attacks, the symptoms will improve yet repeated attacks result in a sensorineural hearing loss that worsens over time.
Whilst the disease will burn out eventually with time, permanent sensorineural hearing loss can remain.
Investigation and Management
Otoscopy will show a normal ear drum, audiometry will show a low frequency sensorineural hearing loss, and tympanometry will show type A (normal). In acute attacks, the vertigo and nausea symptoms can be reduced by a short course of prochlorperazine (a vestibular sedative), given either buccal or intramuscular.
Some conservative measures have been suggested to aim to reduce attack frequency such as lifestyle advice (reducing salt or avoiding chocolate and caffeine) and regular betahistine medication.
If attacks persist despite prophylaxis, surgical intervention may be warranted. This can include intratympanic gentamicin injections, intratympanic steroid injections, endolymphatic sac destruction, or labyrinthectomy (now rarely performed).
Vestibular Neuronitis
Vestibular neuronitis is inflammation of the vestibular nerve, resulting in vertigo that typically lasts days but can last weeks to months. Most cases are due to a viral infection, with a upper respiratory tract infection preceding its onset in half of cases.
Clinical Features
Symptoms will be sudden onset and severely incapacitating, nearly always associated with nausea and vomiting.
On otoscopy, the ear drum will be normal and a horizontal nystagmus will be present when examining the eyes. Neurological examination will be unremarkable and the hearing for these patients will be normal.
Whilst most cases resolve fully within a week; long-term vestibular deficit after the acute episode can lead to unsteadiness over a period of weeks whilst the brain compensates for this.
Investigation and Management
In an acute presentation of dizziness, assessment of a central neurological cause is essential, especially for posterior circulation stroke. Initially this typically involves CT head imaging and, if any uncertainty persists, a subsequent MRI head scan.
Once diagnosed, however, most patients can be managed at home. During the acute episode, a patient may require vestibular sedatives (to be stopped after the acute episode), also considering intravenous fluids if the patient becomes dehydrated from vomiting.
If there are persistent problems due to vestibular hypofunction, then the patient may require longer term vestibular rehabilitation via Cawthorne-Cooksey exercises.
Key Points
- Vertigo can be divided into central and otological causes
- Balance disorders can be caused by a wide range of multifactorial and medical issues such as cardiac or metabolic disorders, especially a posterior circulation stroke in the acute setting
- Main otological causes include Benign Positional Paroxysmal Vertigo, Meniere’s Disease, and Vestibular Neuronitis
- BPPV symptoms last second to minutes, Meniere’s Disease symptoms last minutes to hours, and Vestibular Neuronitis symptoms last days to weeks.