Introduction
The diagnosis of brainstem death is relevant to a number of clinical situations and unfortunately is a commonly performed test in many critical care units.
Brainstem death can be defined as the absence of brainstem reflexes, motor responses, and respiratory drive in a deeply unconscious patient with an irreversible widespread brain lesion of a known cause and no contributing metabolic derangements.
Brainstem death is different to persistent vegetative state (where the patient is also in an irreversible unconscious state) as brainstem dead patients will not survive without respiratory support. Even with ventilatory support, brainstem dead patients will continue to deteriorate and eventually develop multi-organ failure due to loss of biological function
Timely identification of brainstem dead patients is important, as whilst there is no possibility of recovery, it may allow for appropriate referral for organ donation.
This article aims to outline the aspects of brainstem death and the process involved in confirming the diagnosis. It focuses predominantly on UK practice, criteria for assessment and the procedure of testing may vary between countries
Criteria for Assessment Brainstem Death
There are certain preconditions that must be fulfilled and potentially reversible causes excluded prior to formal brainstem testing.
Brainstem testing in the UK should be performed by two qualified doctors, both of whom are competent with the procedure, have full registration with the GMC for > 5 years, and one is a consultant.
The tests should be performed by both doctors together and successful completion is required on two separate occasions.
Preconditions and Exclusion Criteria
Any patient considered for potential brainstem testing should be (1) deeply unconscious (2) apnoeic (3) mechanically ventilated. There should also be certainty that the patient has sustained an irreversible brain damage of known cause.
It is also essential to exclude or correct any reversible causes present that may account for the patient’s condition, prior to continuing with the testing. These include:
- Sedative drugs
- Includes any unknown drug substances used
- Endocrine abnormalities (usually can be excluded from the history)
- Includes any known thyroid or adrenal abnormalities
- Metabolic abnormalities
- Includes potassium, sodium, magnesium, phosphate, and calcium levels
- Hypothermia
- The brainstem is areflexic at temperatures < 28°c
- Cardiovascular instability, with normal target ranges at: pH 7.35 – 7.45, pCO2 < 6.0 kPa, pO2 > 10 kPa, and Mean Arterial Pressure > 60 mmHg
Brainstem Testing
These tests are performed after physicians have confirmed that the patient satisfies the preconditions and has no reversible causes of coma.
All tests should be performed twice and time of brainstem death recorded upon completion of the first set of tests. Both brainstem reflex tests and apnoea tests should be recorded (although not all clinicians perform the latter for every case).
Electroencephalogram (EEG) and CT imaging often help the clinician in the overall picture, however do not form any part of the criteria in diagnosis of brainstem death.
Brainstem Reflex Testing
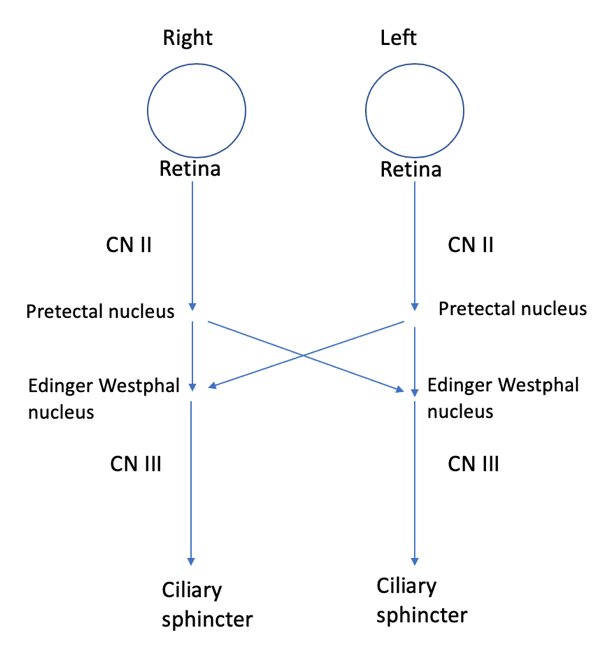
Pupillary Light Reflex
The afferent nerve is CN II, the Edinger Westphal nucleus in the midbrain is the involved brainstem nuclei, and the efferent nerve is CN III.
The test is performed by a bright light being shone into each pupil, testing for both direct and consensual reflexes. The response in brainstem death is the absence of pupillary constriction.
Corneal Reflex
The afferent nerve is CN V1, the trigeminal and facial nuclei in the pons are the involved brainstem nuclei, and the efferent nerve is CN VII.
The test is performed by cotton wool being used to lightly brush the cornea, testing direct and consensual blinking reflexes. The response in brainstem death is the absence of blinking.
Oculo-vestibular Reflex
The afferent nerve is CN VIII, the vestibular and abducens nuclei in the pons and oculomotor nuclei in the midbrain are the involved brainstem nuclei, and the efferent nerves are III and VI (to the medial and lateral rectus muscles).
Otoscopy is initially used to check external auditory canal is clear and tympanic membrane intact. The test is then performed by placing the patient with their head up and 30-50 mL of ice cold saline instilled into the external auditory meatus over 1 minute (both sides should be tested separately). The response in brainstem death is the absence of eye movement towards the side of saline infiltration.
Pain Stimulus
The afferent nerve is CN V, the trigeminal and facial nuclei in pons are the involved brainstem nuclei, and the efferent nerve is CN VII.
The test is performed by a painful stimulus to supra-orbital ridge and the response in brainstem death is the absence of grimacing in response to pain.
Gag Reflex
The afferent nerve is CN IX, the spinal nucleus of V and nucleus ambiguus in medulla oblongata are the involved brainstem nuclei, and the efferent nerve is CN X.
The test is performed by a spatula used to stimulate the pharynx at base of tongue/soft palate. The response in brainstem death is the absence of gag or through elevation of soft plate and pharyngeal contractions.
Cough Reflex
The afferent nerve is CN X, multiple nuclei forming a ‘cough centre’ in medulla oblongata are the involved brainstem nuclei, and the efferent nerve is CN X.
The test is performed by a bronchial catheter being passed to the carina. The response in brainstem death is the absence of a cough.
Apnoea Test
The apnoea test should only be performed after demonstration of absent brainstem reflexes. The test aims to demonstrate brainstem death by producing an acidaemic respiratory stimulus (pH < 7.4) without inducing hypoxia or cardiovascular instability.
Prior to the test, the absence of spontaneous respiratory effort should be confirmed. Various methods for the apnoea test have been described, however one such method includes:
- Reducing minute ventilation until pCO2 reaches 6.0kPa, pH is 7.4, and oxygen saturations above 95%
- Observing for 5 minutes for any respiratory activity
- Demonstrating an increase in pCO2 > 0.5 kPa using arterial blood gas measurements
Once the test has been completed, the ventilator should be reconnected, the correct acid-base status restored, before the repeat test is then performed.
Key Points
- Brainstem death can be defined as the absence of brainstem reflexes, motor responses, and respiratory drive in a deeply unconscious patient with an irreversible widespread brain lesion of a known cause and no contributing metabolic derangements
- Any patient considered for potential brainstem testing should be (1) deeply unconscious (2) apnoeic (3) mechanically ventilated; there should be certainty that the patient has sustained an irreversible brain damage of known cause
- Brainstem testing in the UK should be performed by two qualified doctors, both of whom are competent with the procedure, have full registration with the GMC for > 5 years, and one is a consultant
- All tests should be performed twice and time of brainstem death recorded upon completion of the first set of tests; both brainstem reflex tests and apnoea tests should be recorded