Introduction
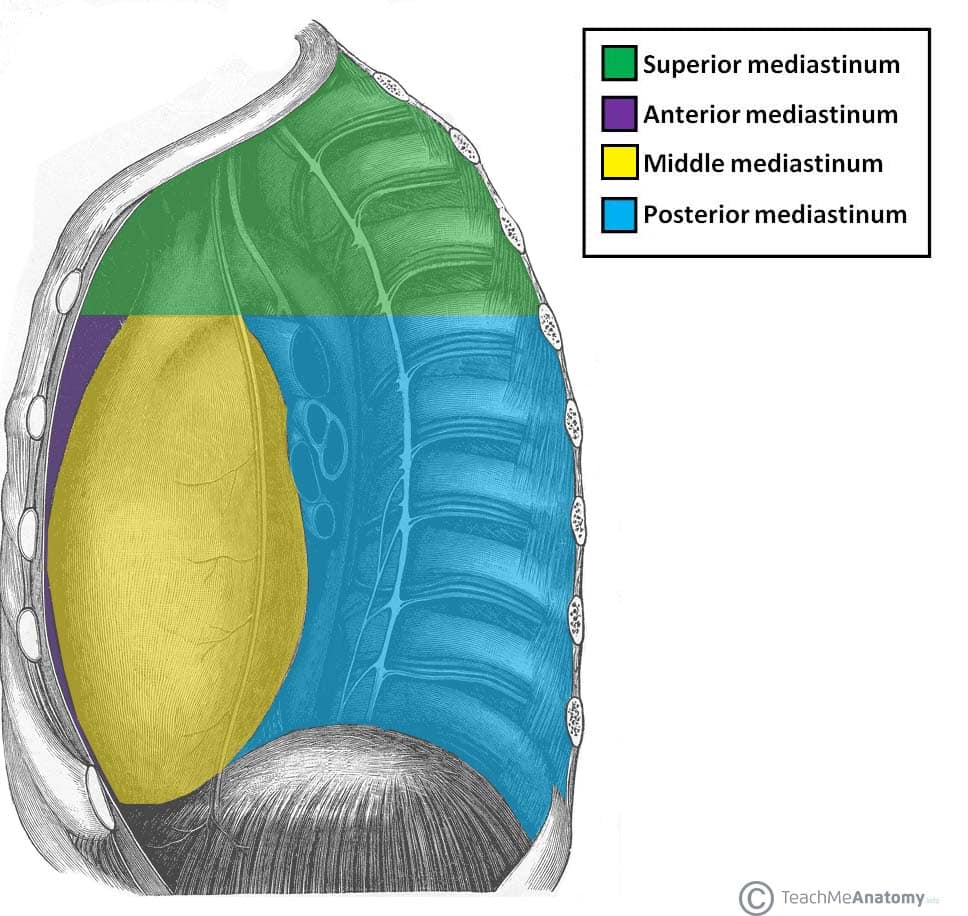
The mediastinum is a space in the centre of the thoracic cavity which contains the heart, thymus, great vessels, part of the oesophagus and trachea, and lymphatics (Fig, 1). Mediastinal tumours refer to tumours that arise from within this space.
Outside of visceral tumours, common types of mediastinal tumour in adults include thymoma, lymphoma, and germ cell tumours*, which will be discussed further in this article. All mediastinal tumours should be discussed at a multi-disciplinary team (MDT) meeting for appropriate investigation and management to be sorted.
A third of adult patients with mediastinal tumours are asymptomatic. Symptomatic patients with mediastinal tumours can present with dyspnoea, persistent cough, symptoms of SVC obstruction (facial swelling, respiratory distress), or nerve compression (such as Horner’s syndrome or recurrent laryngeal nerve compression)
The investigation for mediastinal tumours varies, however often CT imaging +/- mediastinoscopy and biopsy (typically fine-needle aspiration) form the mainstay of investigation.
*These pathologies are located in the anterior mediastinum, the area in front of the pericardium and heart, whilst posterior mediastinal masses tend to be neurogenic in nature and are more common in children
Thymoma
Thymic tumours can be subdivided into either thymomas or thymic carcinomas, depending on their malignant potential (Table 1). Thymomas are the most common mass of the anterior mediastinum, appearing radiologically as small well-circumscribed masses (Fig. 2).
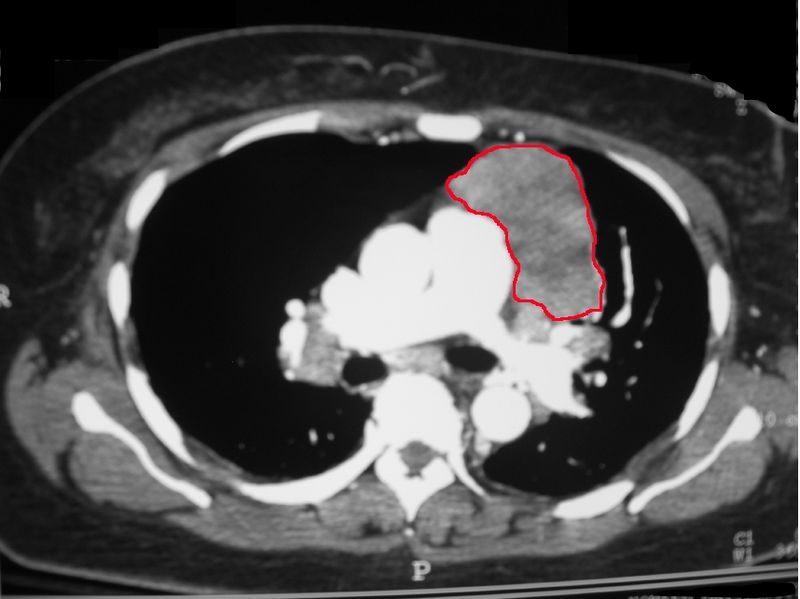
Figure 2 – A CT chest showing a large thymoma in the left anterior mediastinum
Patients can present with dyspnoea, haemoptysis, chest pain, or SVC syndrome. Thymomas have a well-known association with myasthenia gravis (MG), presenting as a paraneoplastic syndrome.
The management of thymoma is surgical excision, which is performed typically via a median sternotomy incision. The excision should aim to cover a wide area, including the whole thymus as well as surrounding areolar fatty tissue, to remove all possible ectopic thymomas.
|
WHO Classification |
Type of Thymic Tumour |
|
| Type A | Medullary thymoma | Thymoma |
| Type AB | Mixed thymoma | |
| Type B1 | Predominantly cortical thymoma | |
| Type B2 | Cortical thymoma | |
| Type B3 | Well-differentiated thymic carcinoma | Thymic carcinoma |
| Type C | Thymic carcinoma | |
Table 1 – Classification of Thymic Tumours
Lymphoma
Lymphomas are malignant proliferations of lymphocytes, which accumulate in the lymph nodes, and are a common cause of mediastinal masses. Lymphoma can be broadly divided into Hodgkins lymphoma and non-Hodgkins lymphoma; this article discusses lymphoma specific to the mediastinum, however lymphoma may occur anywhere in the body
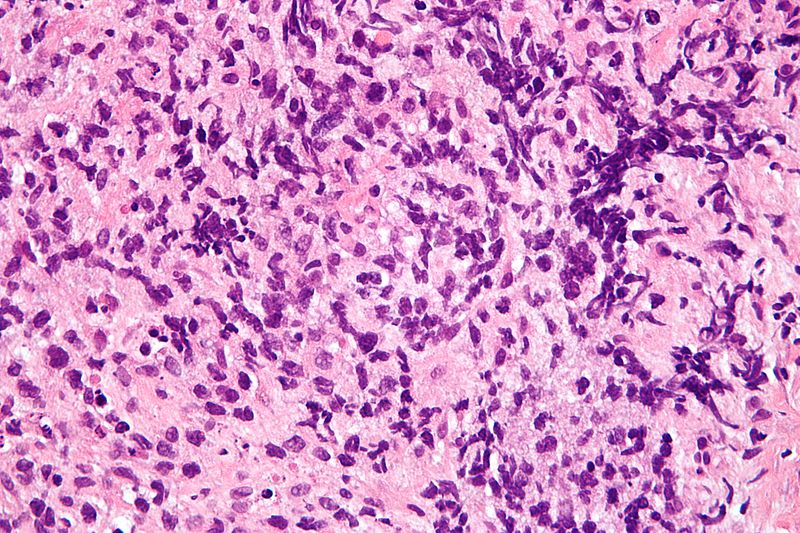
Figure 3 – Histology of a primary mediastinal large B-cell lymphoma from core biopsy
In the mediastinum, lymph nodes can be divided into groups; the most common nodes to be affected in lymphoma are the prevascular and paratracheal nodes, which are found in the superior mediastinum.
Patients with lymphoma present with lymphadenopathy and constitutional symptoms (fever, chills, weight loss, night sweats). Lymphoma symptoms specific to the mediastinum include chest pain, cough, dyspnoea, and hoarseness of voice (secondary to recurrent laryngeal nerve compression).
Ann Arbor Staging System
Lymphoma can be staged using the Ann Arbor staging system:
- Stage 1 – Confined to single lymph node region
- Stage 2 – Involvement of ≥2 lymph node regions the same side of the diaphragm
- Stage 3 – Involvement of lymph nodes on both sides of the diaphragm
- Stage 4 – Involvement of extranodal sites (e.g. liver or bone marrow)
- Modifying features – A = no symptoms; B = fever, night sweats, or weight loss >10% in 6 months
Treatment is often by chemotherapy +/- radiotherapy, with an aim for cure even in stage 4 disease. Survival rates are determined by disease stage, disease grade, and patient factors.
Germ Cell Tumour
Germ cell tumours (GCT) generally present from the 2nd to the 4th decade of life and include teratoma, seminomatous GCT, and non-seminomatous GCT.
The mediastinum is the most common extragonadal site for GCTs, with 60% of mediastinal GCTs occurring in the anterior compartment. Teratomas are the most common mediastinal GCT.
Surgical excisions are generally the treatment of choice for mediastinal GCTs, however malignant teratomas will often require adjuvant radiotherapy +/- chemotherapy.
Key Points
- Common types of mediastinal tumour in adults include thymoma, lymphoma, and germ cell tumours
- A third of adult patients with mediastinal tumours are asymptomatic; symptomatic patients with mediastinal tumours can present with dyspnoea, persistent cough, symptoms of SVC obstruction, or nerve compression
- The investigation for mediastinal tumours varies, however the majority require CT imaging and biopsy