Introduction
- Introduce yourself to the patient
- Wash your hands
- Briefly explain to the patient what the examination involves
Approach the examination in a systematic way, starting from the outer parts of the ear before moving to the inner parts of the ear; be prepared to be instructed to move on quickly to certain sections by any examiner.
Pinna and Post Auricular Area
Inspect the pinna and the mastoid:
- Obvious deformities or abnormal cartilaginous fragments
- Scars or skin changes
- Including for skin malignancies
- Signs of inflammation
- An inflamed mastoid may push the pinna forward
Palpate the lymph nodes and pinna, specifically:
- Pre- and post-auricular lymph nodes
- Tragus
- Tragal tenderness is a sign of otitis externa

Figure 1 – A basal cell carcinoma located on the posterior aspect of the outer ear
External Ear Canal
Inspect the outer aspect of the external ear canal using the otoscope as a light source
Gently straighten out the ear canal by pulling the external ear superiorly and posteriorly
Look for signs of:
- Wax or a foreign body
- Skin changes or erythema
- Discharge
Tympanic Membrane
Hold the otoscope like a pen between thumb and index finger, left hand for left ear and right hand for right ear, resting your little finger on the patient’s cheek – this acts as a pivot.
Gently straighten out the ear canal by pulling the external ear superiorly and posteriorly
For a normal tympanic membrane, you should be able to observe*:
- Lateral process of malleus
- Cone of light
- Pars tensa and pars flaccida
*The cone of light can be used to orientate; it is located in the 5 o’clock position when viewing a normal right tympanic membrane and in the 7 o’clock position for a normal left tympanic membrane.
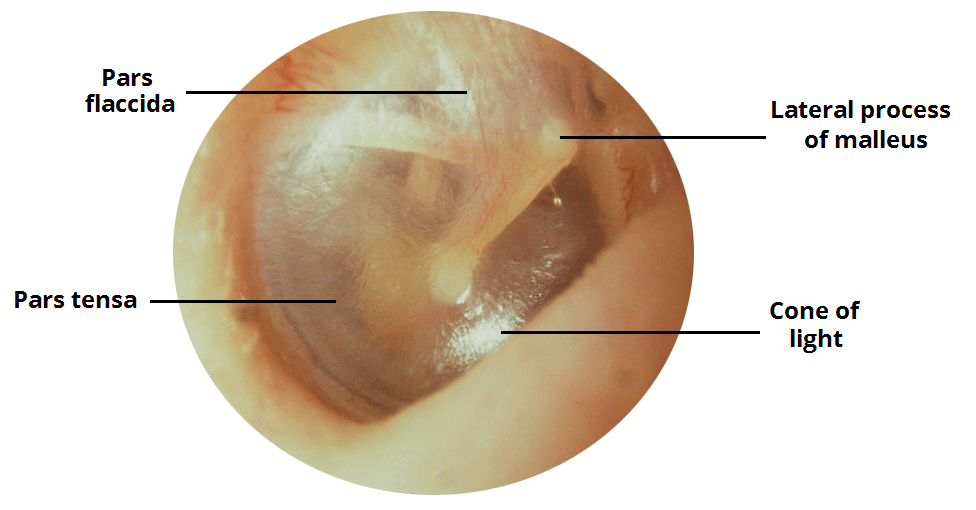
Figure 2 – A normal right tympanic membrane
For an abnormal tympanic membrane, common signs may include:
- Perforations
- Tympanosclerosis
- Red and bulging membrane
- Retraction of the membrane
Ensure to check the function of the facial nerve
Assessment of Hearing
Rinne Test
Strike the tuning fork (512Hz) against your elbow and place against the mastoid process (bone conduction), then once patient stops hearing it, hold it near the external ear canal (air conduction)
- For normal hearing or sensorineural hearing loss, air conduction is heard better than bone conduction (Rinne positive)
- For conductive hearing loss, bone conduction is heard better than air conduction (Rinne negative)
Weber Test
Strike the tuning fork (512Hz) against your elbow and place on the patient’s forehead in the midline. Ask the patient whether the sound is heard in the midline or has lateralised
- For normal hearing, the sound is heard in the midline
- For conductive hearing loss, the sound is loudest on the ipsilateral side to the hearing deficit
- For sensorineural hearing loss, the sound is loudest on the contralateral side to the hearing deficit
Completing the Examination
Remember, if you have forgotten something important, you can go back and complete this.
To finish the examination, stand back from the patient and state to the examiner that to complete your examination, you would like to perform a:
- Tympanogram
- Pure tone audiometry

