Introduction
Cysts of the liver are a relatively common condition, most commonly through incidental identification on routine imaging.
Whilst the majority of cases are simple cysts, a small number are caused by malignancy or infection, therefore careful assessment of each case is required.
In this article, we will discuss the varying types of cystic liver disease, along with the necessary investigations required and management options available.
Simple Cysts
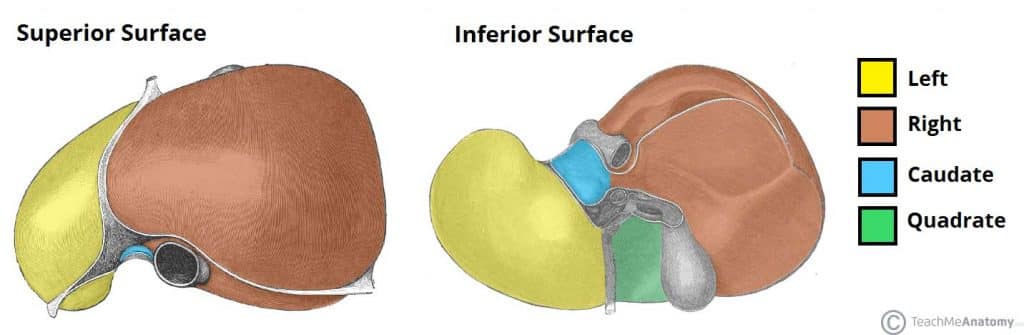
Simple liver cysts are simple fluid-filled epithelial-lined sacs within the liver, most commonly occurring in the right lobe of the liver. They are relatively common, with a prevalence of 2.5-5%, with an increasing incidence with age and are slightly more common in females.
Most are thought to be due to congenitally malformed bile duct cells failing to connect to the extrahepatic ducts, which leads to a local dilatation filled with a bile-like fluid, of varying size.
Clinical Features
Simple cysts are normally asymptomatic and often detected incidentally on imaging.
Around 10-15% of patients experience symptoms due to mass effect, with symptoms including visible epigastric swelling, abdominal pain, nausea, and early satiety. As expected, larger cysts are more likely to be symptomatic.
Simple liver cysts may also cause acute pain if bleeding into the cysts occurs, which can result in a rapid increase in their size (albeit rarely of sufficient volume to cause haemodynamic instability).
Investigations
Patients liver function tests are typically normal, although a small number of patients may have a raised ALP or GGT. Tumour markers CEA and CA19-9 can also be mildly elevated in some cases.
Ultrasound remains the imaging modality of choice for the diagnosis of liver cysts. Simple cysts are characteristically anechoic, well-defined, thin-walled (often imperceptible), oval or spherical lesions with no septations, and strong posterior wall acoustic enhancement.
If any worrisome features are evident, such as septae, irregular borders, or intra-cystic echogenicity, then further investigation with MRI imaging may be indicated.
Management
Most cysts require no intervention, though for cysts >4cm in size, follow-up ultrasound imaging is recommended at regular intervals post-detection, to monitor for any significant growth.
If the size of the cyst remains unchanged after 2-3 years, no further scans are required (unless the patient becomes symptomatic).
If the patient is symptomatic or the diagnosis is uncertain, further intervention may be warranted. Options include ultrasound-guided aspiration or laparoscopic de-roofing of the cyst, with the latter having lower rates of failure and recurrence.
Caroli Disease
Caroli disease is a rare form of congenital cystic disease, whereby there is a segmental dilation of large intrahepatic bile ducts, appearing as cysts on imaging. When scarring is seen at the same time, Caroli Syndrome is diagnosed.
The disease is mediated by the same gene responsible for autosomal recessive polycystic kidney disease (ARPKD) and carries an 5-10% risk of malignant transformation. Depending on disease location, management is by liver resection or transplant.
Polycystic Liver Disease
Polycystic liver disease is characterised by the presence of ≥20 cysts within the liver parenchyma, each of which are ≥1cm in size.
They are almost invariably caused by one of the two following autosomal dominant conditions:
- Autosomal dominant polycystic kidney disease (ADPKD)
- Caused by mutations in the PKD1 (chromosome 16) and PKD2 (chromosome 4) genes, whereby 10-60% of patients will also develop have liver cysts (the most common extra-renal manifestation of ADPKD)
- Autosomal dominant polycystic liver disease (ADPLD)
- Caused by mutations in the PRKCSH (chromosome 19) or SEC63 (chromosome 6) genes; patients with this genotype will not have any renal involvement
Mutations in these genes result in aberrant ductal plate configurations during liver embryogenesis. Importantly, these structures are not connected to the intrahepatic bile ducts and so do not drain, leading to dilatation and eventual cyst formation as they progressively fill with bile-like fluid.

Figure 2 – A CT scan showing a patient with polycystic liver disease, in axial and coronal views
Clinical Features
The majority of patients with polycystic liver disease are asymptomatic, with symptoms mainly arising as a result of localised compression.
Those with symptoms will often present with abdominal pain as the cysts grow in size. Localised mass effect can further result in nausea and early satiety. In many cases, hepatomegaly will be evident on examination.
Any concurrent renal disease may also present with additional renal issues. Severe disease can lead to portal hypertension and ascites formation, even with end-stage liver disease.
Investigations
Patients will typically have normal liver function tests (ALP can become raised in a small proportion); renal function can be affected in those with renal cysts too.
Definitive diagnosis is via ultrasound imaging, which can show a liver containing multiple cysts, with ≥20 at least 1cm in size, all of which have the same sonographic characteristics as simple cysts
Management
Patients with asymptomatic polycystic liver disease require monitoring only initially, however the progressive nature of the condition means that many require some form of intervention eventually. Some evidence suggests that somatostatin analogues can be trialled for symptomatic relief in certain patients, acting to reduce cyst volume
The main indications for intervention for patients with polycystic liver disease are (1) intractable symptoms (2) inability to rule out malignancy on imaging alone (3) prevention of malignancy. Options include:
- Laparoscopic de-roofing of cysts is the preferred technique in those experiencing symptoms or for whom there is evidence of compression of surrounding structures; it is generally only helpful where a dominant cyst(s) can be identified and targeted
- Due to the diffuse nature of the disease, liver resection is rarely indicated but in severe disease, liver transplantation may be warranted
- US-guided aspiration may provide temporary relief in patients experiencing pain due to cyst size, although this is not routinely performed due to fluid re-accumulation
Cystic Neoplasms
True cystic neoplasms of the liver are rare, accounting for <5% of all liver cysts. The most common subtype are cystadenomas (non-invasive mucinous cystic neoplasms), which are premalignant lesions. They develop as a result of abnormal proliferation of biliary epithelium, however can undergo malignant transformation into cystadenocarcinomas in around 10% of cases.
Clinical Features
As with other hepatic cysts, patients are commonly asymptomatic. Cystic neoplasms will grow slowly, typically 1-2mm per year and if symptoms do develop, they may do so insidiously. Symptoms are the same as seen with simple cysts.
Investigations
Patients will typically have normal liver function tests, although ALP, CEA, and CA19-9 can all become mildly elevated. Importantly, ultrasound imaging will often be able to differentiate between simple cysts and more complicated cystic lesions.
As such, CT imaging or MR imaging with contrast should be performed on all patients in whom a cystic neoplasm is suspected for further delineation (see below) +/- evidence of metastasis (cystadenoma tend to be multiloculated, with thick enhancing septations)
Aspiration or biopsy should be avoided if a cystic neoplasm is suspected as this can result in potential peritoneal seeding of the malignancy (if done, the aspirate is typically a mucinous fluid).
Suspicious Features on Imaging
There are several features that can be seen on imaging for liver cysts that can suggest a sinister pathology:
- Suspicious for malignancy – (1) septations (2) wall enhancement (3) nodularity
- Suspicious for abscess – (1) debris within the lesion (2) loculation (may also suggest malignancy)
- Suspicious for hydatid cyst – (1) calcification (2) “daughter cysts” around the main lesion
Management
Liver lobe resection is the treatment of choice for both cystadenomas and cystadenocarcinomas, with the samples only then sent for histopathology to confirm the diagnosis.
Cyst deroofing and aspiration should be avoided due to the high risk of recurrence and the underlying risk of malignant transformation.
Hydatid Cysts
Hydatid cysts, or Echinococcal cysts, result from infection by tapeworms of the genus Echinococcus, most commonly Echinococcus granulosus or Echinococcus multilocularis, and has a global distribution (highest in South America, North Africa and Central Asia)
Echinococcus mature in a definitive host, most commonly dogs, after eating infected meat. Eggs are produced in the animal’s gut and excreted where they can be ingested accidentally by an intermediate host, such as humans.
The eggs hatch to release oncospheres that penetrate the gut lining and migrate in the blood to the liver, although they can also infect the lungs and brain, and form hydatid cysts. These cysts enlarge and may produce daughter cysts, but do not mature to adult form unless ingested by a definitive host.

Figure 3 – A opened hydatid cyst in the liver of a sheep
Clinical Features
Cysts may only grow at a rate of a couple of millimetres per year. As a result, theycan remain asymptomatic and undetected for many years. Hydatid cysts are locally destructive, resulting in potential disruption to the bile ducts.
Most patients with symptoms will report a vague abdominal pain, caused by the mass effect on surrounding structures (or less commonly due to cyst rupture). As with other liver cysts, localised mass effect can further result in nausea and early satiety.
Rarely, patients can present in anaphylaxis if the cyst ruptures into the thorax or intraperitoneally, which can be fatal. Cyst rupture may also lead to disseminated cystic disease.
Investigations
Patients will typically have normal liver function tests, whilst the full blood count can show an eosinophilia. Echinococcal antibody titres are positive in 80% of those with the disease.
Ultrasound imaging will show calcified spherical lesion(s) with multiple septations, either anechoic or containing snowflake-like bodies.
Further assessment can be performed via CT imaging or MR imaging, to allow proper definition of the anatomical relations of the cyst(s) and any biliary involvement.
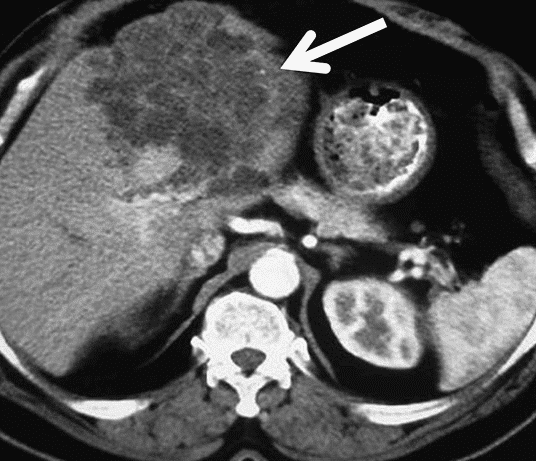
Figure 4 – CT scan demonstrating polycystic echinococcosis affecting the left lobe of the liver
Management
The primary treatment for hydatid cysts is surgical with complete cyst excision (or deroofing when the cyst is adjacent to vital structures).
Radiological drainage and injection of scolecidal agent (the PAIR technique) is also an option in specialist centres (to avoid dissemination of parasites at surgery, hypertonic saline is often infected to the cyst at the start of the procedure)
Medical management is used as an adjunct to surgical therapy or in those with disseminated hydatid disease. The specific regime of anti-microbials varies, however use of albendazole + mebendazole + praziquantel is one possible option.
Aspiration is not recommend in those with suspected hydatid cysts, as rupture may cause an anaphylactic reaction. If cysts are asymptomatic and inactive, it may be possible to simply monitor them.
Key Points
- Most cystic disease of the liver is asymptomatic and is identified incidentally on routine imaging
- Indications for surgery for cystic liver lesions are (1) intractable symptoms (2) inability to rule out malignancy on imaging alone (3) prevention of malignancy
- Aspiration or biopsy should be avoided if a cystic neoplasm is suspected as this can result in potential peritoneal seeding of the malignancy
- Parasitic cysts are rare but should be excluded and if diagnosed, should be referred to an appropriate specialist management centre