Introduction
Spinal infections are rare, but often serious, whereby bacteria, fungi, or viruses are able to invade the spinal tissues. There are multiple potential sites of infection in the spine (Fig. 1), thus spinal infections form a spectrum of disease.
The most frequently involved spinal segment is the lumbar spine (58%), followed by the thoracic spine (30%)
Vertebral Osteomyelitis
Infection of the vertebral body, also termed spondylitis, is the most common form of spinal infection. Subtypes include pyogenic vertebral osteomyelitis and granulomatous vertebral osteomyelitis (Potts’s disease, caused by tuberculosis).
Discitis
Isolated infection of the intervertebral disc (the nucleus pulposus), however can also spread to adjacent vertebral bodies (termed spondylodiscitis). The condition has a high prevalence in children.
Epidural Abscess
An epidural abscess develops in the space between the dura mater and vertebral column. They more commonly affect those in 5th to 7th decade of life and are more common in males.
Subdural Abscess
A subdural abscess develops in the space between the dura mater and arachnoid mater. The spinal subdural space has no barriers to prevent the spread of infection, so often spinal subdural infections can rapidly expand to involve multiple spinal levels.
Spinal Cord Abscess
Spinal cord abscesses, also termed intramedullary abscesses, are very rare infections that occur around the spinal cord.
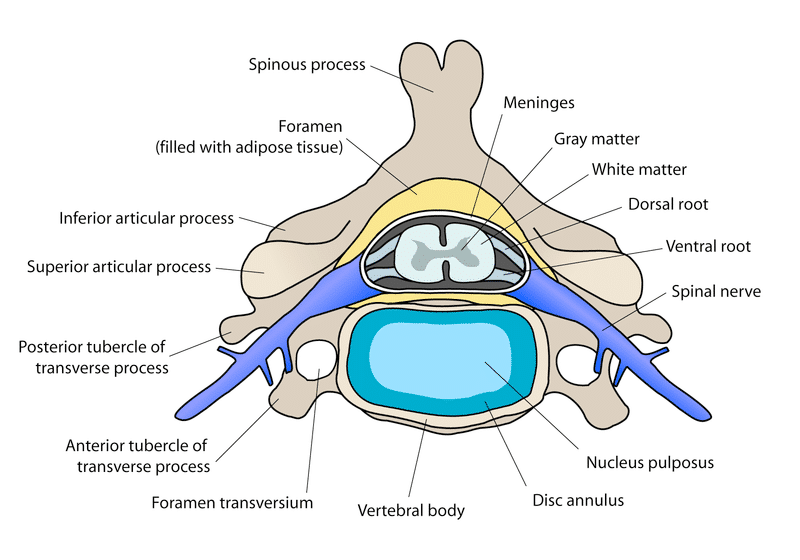
Figure 1 – Anatomical relationship between the vertebrae, intervertebral discs, meninges, and spinal cord
Pathophysiology
There are three main routes by which a pathogen can breach the spinal column, producing a spinal infection:
- Haematogenous spread – most common route, especially for vertebral osteomyelitis, due to rich vascular supply from the anterior spinal artery*
- Direct inoculation – Usually after trauma, spinal surgery, or spinal (such as a lumbar puncture or spinal anaesthesia)
- Adjacent spread – Infected adjacent tissue can allow infection to spread throughout the spine, however this is less common
The most common organisms in spinal infections are bacterial, mainly S. aureus (55–80% of cases) and E. coli.
*This supplies the anterior 2/3rd of the spinal cord and consequently the anterior portion of the spine is where infections most commonly originate
Risk Factors
The main risk factors for spinal infections include intravenous drug use (due to resultant haematogenous spread of pathogens), immunosuppression (including steroid and immunosuppressant use), malignancy, diabetes mellitus, and recent spinal surgery (via direct inoculation)
Clinical Features
The main symptom patients present with for all types of spinal infection is back pain. This is often worse on movement and worse at night. Associated features can include pyrexia and radicular signs, progressing to weakness or paralysis in severe cases.
On examination, patients will be focally tender at the level of infection. In patients reporting neurological compromise, a detailed upper and lower neurological examination, with specific focus on motor and sensory aspects is crucial to elicit the extent of the infected portion of the spine.
Ensure to check for features of spinal cord compression and cauda equina syndrome. Always check for other potential sources of infection that may have seeded to cause any spinal infection (e.g. infective endocarditis)
Differential Diagnosis
For patients presenting with acute back pain, the main differentials to consider include intervertebral disc prolapse, spinal fracture, musculoskeletal injury, or spinal malignancies.
Investigations
Laboratory Tests
Any patient suspected of having a spinal infection should have routine blood tests, including FBC, CRP, U&Es, LFTs, and clotting studies. Due to haematogenous spread, blood cultures should also be performed.
Imaging
Imaging is necessary to pinpoint the location and extent of a lesion. Detection of spondylitis/spondylodiscitis may be difficult or impossible during early infection, especially plain radiographs.
The gold standard investigation to visualise spinal infections is MRI imaging with contrast. MRI can accurately identify the location and type of spinal infection (Fig. 2), and most importantly can determine the involvement of the central canal and spinal cord.
CT imaging cannot show soft tissue pathology as well as MRI imaging, however can be used to determine the extent of any bony involvement (Fig. 3).
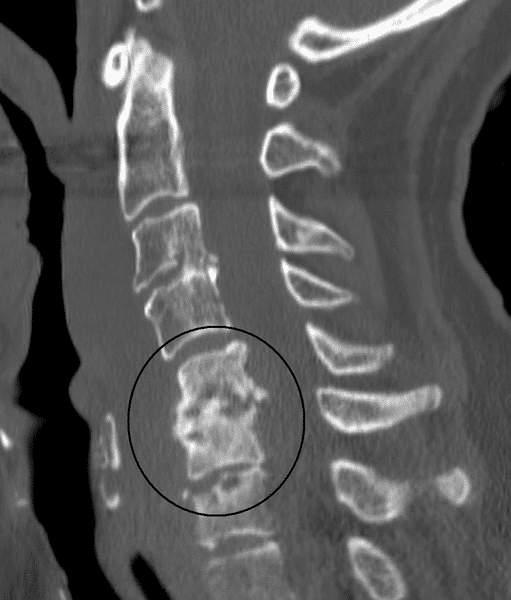
Figure 3 – CT imaging showing associated bone involvement (circled) in a case of discitis
Biopsy
In confirmed cases, CT-guided biopsy is recommended where feasible to obtain samples for both microbiology and histology. This can further help with choice antibiotic, once pathogen sensitivities have been determined.
Management
Spinal infections often require long-term intravenous antibiotic (or antifungal) therapy, which often equates to an extended hospitalisation time for the patient. In approximately 90% of cases, conservative treatment is successful in achieving these goals.
Immobilisation may be recommended when there is significant pain or in cases of spinal instability.
Surgical Intervention
Surgery may be indicated when there is evidence of significant bone destruction (causing spinal instability), the presence of neurological deficits (including spinal cord compression), or a poor response to antimicrobial treatment
The primary goals of surgery in spinal infections are to debride the infected tissue and drain residual pus, and restore spinal stability where possible.
Response to treatment is usually assessed by looking at the patient’s symptoms, inflammatory markers, and repeat MRI imaging at intervals during the treatment period.
Key Points
- Spinal infections are rare but serious infections of the spinal tissues
- Vertebral Osteomyelitis and Discitis are the most common forms
- Gold-standard diagnosis is made via MRI imaging
- Treatment is often with long-term antimicrobial therapy, however surgical intervention may be required in select cases

