Introduction
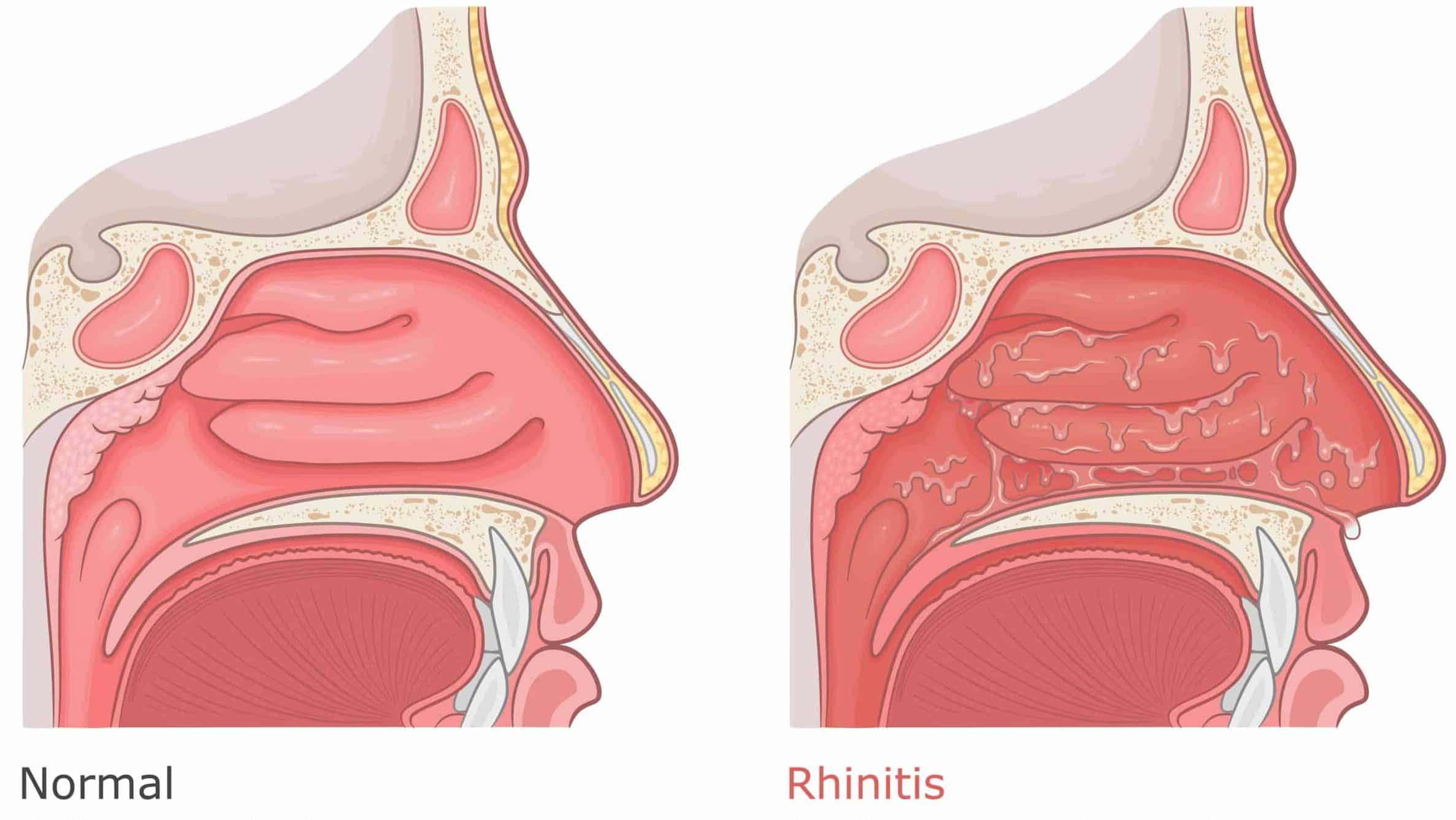
Acute rhinosinusitis is a common condition, affecting 8-15% of the population at any one time. It is characterised by acute inflammation of the mucosal linings of the nasal passage (rhinitis) and paranasal sinuses (sinusitis).
There are a variety of precipitants for acute inflammation of nasal mucosa, such as infection and allergy. Inflammation of mucosa results in blockage of the paranasal sinuses and subsequently can lead to a bacterial infection.
The most common causes are a viral organisms, such as rhinovirus, influenza, or adenovirus, however can also be caused by bacterial organisms, such as S. pneumoniae, H. Influenzae, or M. catarrhalis. Allergic precipitants that can cause acute rhinosinusitis dust, pollen, and cat or dog hair.
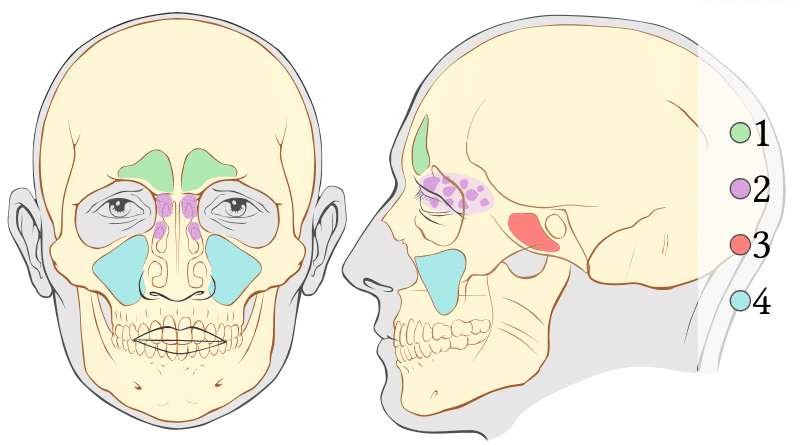
Paranasal Sinuses
Paranasal sinuses are hollow spaces within the bones of the face, arranged symmetrically around the nasal cavity (Fig. 2).
- Frontal sinuses – located within the frontal bone of the skull, the most superior of the paranasal sinuses and are triangular in shape
- Ethmoid sinuses – formed in the ethmoid bone, made up of 3 separate cavities (anterior, middle, and posterior)
- Sphenoid sinuses – situated within the body of the sphenoid bone, opening out into the nasal cavity in an area supero-posterior to the superior cocha
- Maxillary sinuses – the largest of the sinuses, located laterally and slightly inferiorly to the nasal cavities and drain into the nasal cavity via the osteomeatal complex in the middle meatus
Risk Factors
The main risk factors for acute rhinosinusitis include:
- Cigarette smoke exposure (active or passive)
- Air pollution exposure
- Anatomical variations, such as septal deviation, nasal polyps, or sinus hypoplasia
- Atopic disease, such as asthma or hayfever
Clinical Features
Acute rhinosinusitis is distinguished from chronic rhinosinusitis by the duration of symptoms. Symptoms lasting less than 12 weeks are classified as acute rhinosinusitis. Episodes are more common in the winter months.
The diagnosis of acute rhinosinusitis requires the sudden onset of two or more of the following symptoms:
- Nasal obstruction
- Discoloured nasal discharge (either anterior or posterior discharge)
- Facial pain or pressure (usually unilateral over the maxillary or frontal sinus)
- Altered sense of smell
Symptoms that may suggest a bacterial cause include severe local pain, discoloured discharge, fever, or worsening after an initial improvement (post-viral).
Differential Diagnosis
The main differential diagnoses for acute rhinosinusitis include:
- Viral upper respiratory tract infection – symptoms tend to improve with symptomatic treatment within 3-5 days
- Allergic rhinitis – should be suspected where there is a history of allergy or atopy, and symptoms include other allergic features; mucopurulent discharge or loss of sense of smell are unlikely
- Facial pain syndromes – includes diagnosis such as migraines, cluster headaches, or mid-segment facial pain; the absence of other nasal symptoms make these diagnoses more likely
- Nasal foreign body – causes a unilateral mucopurulent discharge or blockage; more common in children
Investigations
The diagnosis of acute rhinosinusitis is typically made on clinical symptoms alone. Imaging, such as a CT scan (Fig. 3), may be required if complications are suspected.
Skin prick testing for allergy might be appropriate in patients with recurrent episodes and symptoms suggested of allergic rhinitis.
Management
Most cases of acute rhinosinusitis cases can be managed in the community, and do not require treatment with antibiotics. The aim of treatment is to reduce inflammation of the nasal mucosa and improve the drainage of the paranasal sinuses.
Initial Management
For uncomplicated acute rhinosinusitis without features of bacterial infection,treatment with analgesia, nasal douche and nasal decongestants will suffice. For those with signs of acute bacterial rhinosinusitis (e.g. purulent discharge or fever*), antibiotics are indicated.
If there is no improvement after 7-14 days of treatment or the presence of red-flag symptoms, referral to ENT services should be considered.
*A common sign of a bacterial infection is “double sickening”, where the patient worsens after a preceding mild phase of illness
Red Flag Symptoms
- Eye signs, including periorbital swelling or erythema, displaced globe, visual changes, ophthalmoplegia.
- Severe unilateral headache, bilateral frontal headache, or frontal swelling.
- Neurological signs or reduced conscious level.
Specialist Management
An ENT specialist will perform nasal endoscopy, to identify any abnormal anatomy or pathology. A culture of any nasal discharge may be warranted for atypical infections.
A CT scan of the paranasal sinuses would show the extent of the disease, as well as identifying complications (see below) and any underlying anatomical abnormalities.
For severe infections or complications, admission might be necessary for treatment with oral steroids, intravenous antibiotics, and the consideration of surgery.
Complications
Potential complications of acute rhinosinusitis include:
- Peri-orbital cellulitis – sinusitis is the commonest cause of orbital cellulitis (Fig. 4)
- Osteomyelitis – infection invading the bone can eventually lead to penetration into the skull vault causing intracerebral complications
- Pott’s puffy tumour – osteomyelitis of the frontal sinus can result in a soft boggy swelling over the overlying tissue on the forehead (Fig. 5)
- Intracranial abscess or venous sinus thrombosis
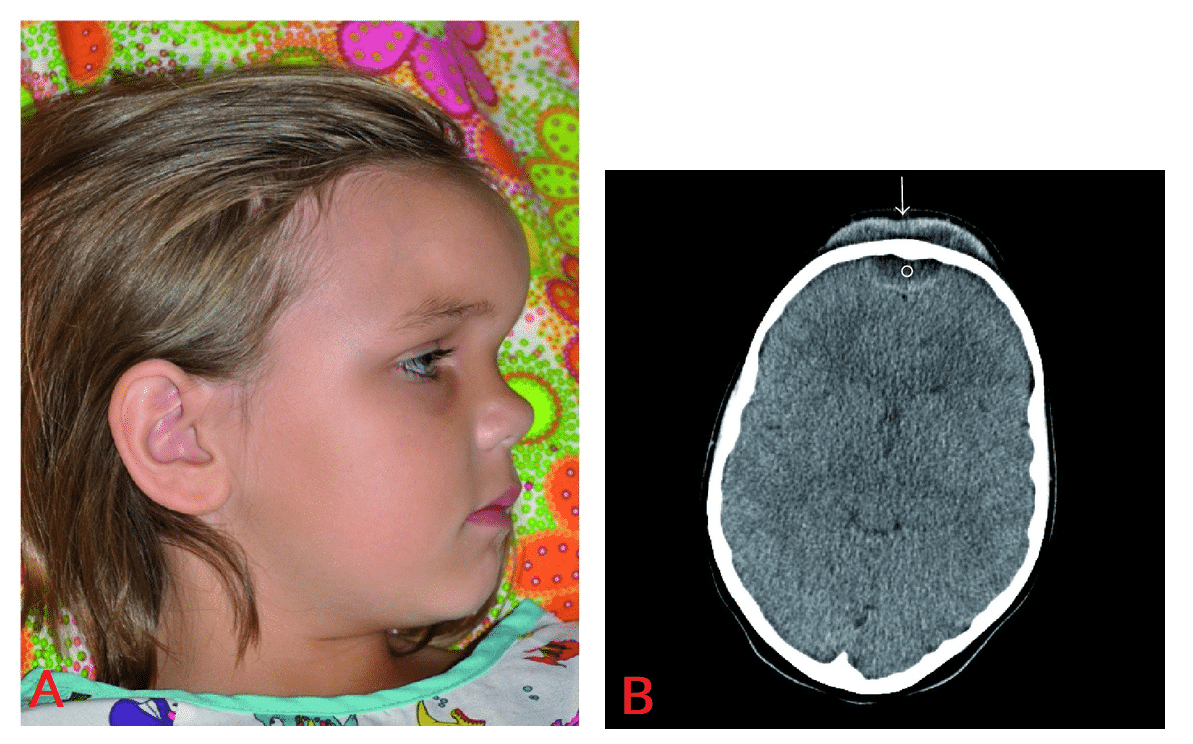
Figure 5 – Pott’s puffy tumour. A) Child demonstrating a notable amount of fullness over the area corresponding to the frontal sinus. B) Axial CT of the brain demonstrating subperiosteal (arrow) and epidural abscesses (circle).
Key Points
- Acute rhinosinusitis is inflammation of the mucosal linings of the nasal passage and paranasal sinuses
- Symptoms include nasal obstruction, nasal discharge, facial pain or pressure, or an altered sense of smell
- Most cases can be diagnosed clinically and can be managed conservatively (antibiotics are not routinely required)
- If no improvement after treatment or there is the presence of red-flag symptoms, referral to ENT services is warranted