Introduction
Pancreas transplantation (PT) is indicated for the treatment of patients with diabetes mellitus (typically type 1 diabetes mellitus), acting to restore glycaemic control and reduce the impact of diabetes-related complications.
Even though PT is not a lifesaving operation, it is performed due to the significant increase to patient quality of life, through halting of the progress of diabetic complications, cessation of daily insulin injections, and overall improved life expectancy. Currently, the overall 5-year post-PT patient survival rate is approximately 93%. 5-year pancreas transplant graft survival is 84%.
Pancreatic Islet Transplantation
It is worth noting that pancreatic islet transplantation can also be used in diabetes mellitus (DM) patients with or without simultaneous renal transplantation. Whilst it is a less invasive and risky procedure, it comes with signficantly lower rates of long-term insulin independence therefore is only performed in very select patients.
Types of Pancreas Transplantation
The types of PT are Simultaneous Pancreas and Kidney (SPK), Pancreas After Kidney (PAK), and Pancreas Transplant Alone (PTA). Donor-recipient matching is based on ABO and HLA-based compatibility.
The SPK transplantation accounts approximately for 90% of all PTs, offering better long-term patient survival than kidney transplant alone.
PTA transplantation is offered for patients without significant renal disease but with life-threatening complications of diabetes (e.g. hypoglycaemic unawareness or uncontrolled BMs)*, whilst the PAK transplantation is usually seen in those following a living donor kidney transplantation.
*The patient may still require a kidney transplant in the future
Indications
Patients with DM* who have progressed to end-stage renal disease (eGFR < 15 ml/min, or dialysis is anticipated within 18 months) or experience life-threatening DM-related complications are candidates for surgery. Rarely pancreas transplant can be performed for cystic fibrosis-related pancreatic disease.
*Historically, only type 1 DM patients were considered for PT, however in select type 2 DM patients, PT has led to significant improvement in glycaemic control
Contraindications to solid-organ pancreas transplantation can be divided into absolute and relative (Table 1). Cardiovascular disease is the main determinant of recipient morbidity and mortality after PT. The assessment for cardiovascular disease is therefore of paramount importance before listing and while on the waiting list.
|
Absolute |
Relative |
|
|
Table 1 – Contraindications to pancreas transplantation
Surgical Techniques
Donor Retrieval Procedure
Full exposure of the abdomen is obtained via laparotomy, with the bowel mobilised to gain full access to the retroperitoneum, the distal abdominal aorta tied, and the organs perfused with cold perfusion solution.
The pancreas is removed with the spleen and duodenum attached. The harvested pancreas will eventually end up with three arterial stumps (the SMA off the aorta, the splenic artery off the coeliac trunk, and the gastroduodenal artery off the common hepatic artery) and one venous stump (the portal vein). The mesenteric root is stapled.
The pancreas is removed and placed on ice, inspected for quality, fattiness, fibrosis and evidence of any damage from the retrieval. The organ is packed in preservation solution and transported to the recipient centre for implantation within 12 hours.
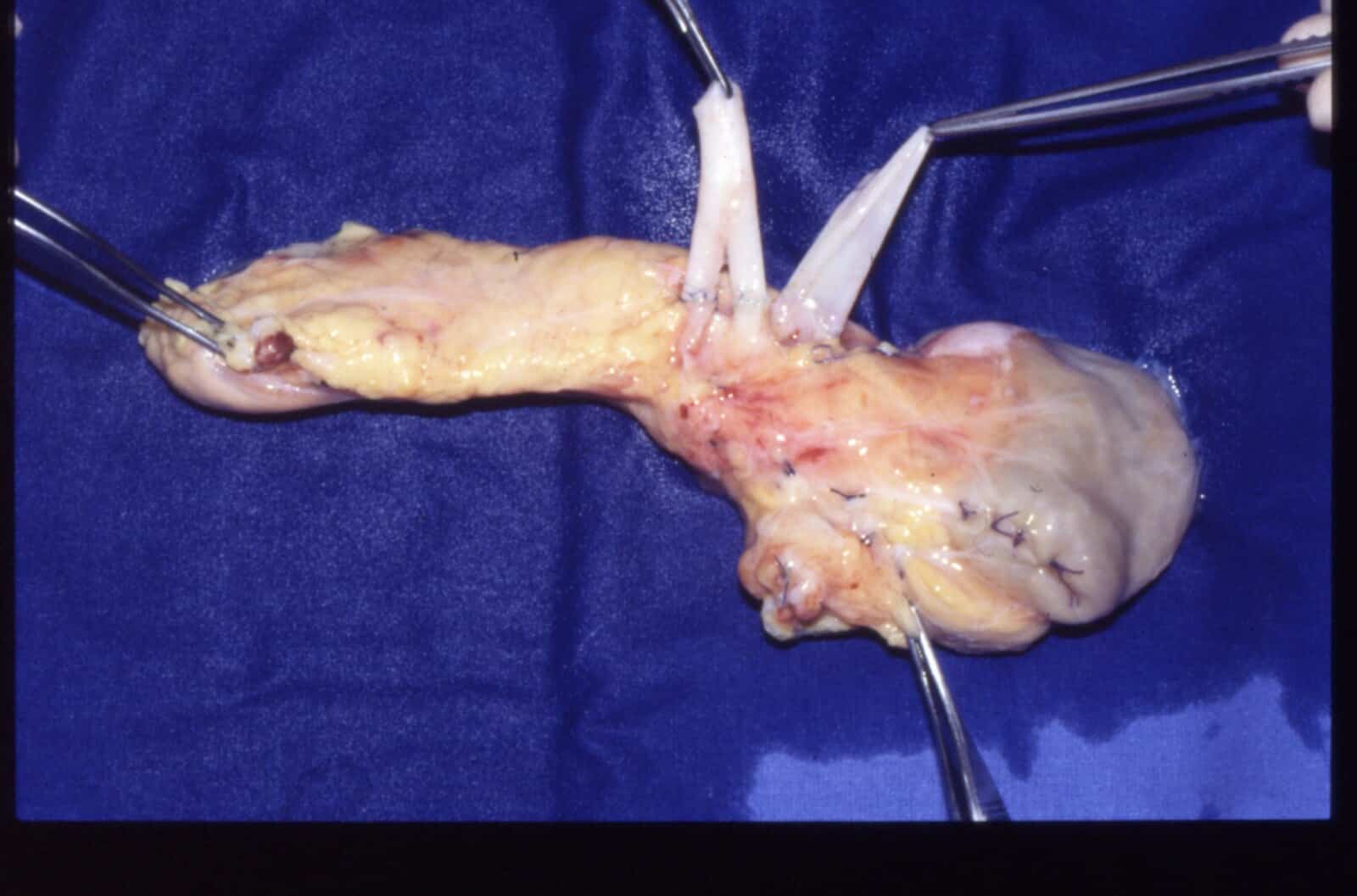
Figure 2 – A pancreas transplant ex-situ, awaiting implantation
Recipient Procedures
The gastroduodenal artery is transfixed and the donor’s common arteries are used as a Y-graft is used to connect the donor SMA and splenic arteries into one arterial stump. The native recipient pancreas is not removed.
A recipient midline laparotomy is performed. The graft is placed in the the retroperitoneum (similar to a kidney transplant), with the graft arterial Y-graft implanted on the right common iliac artery and the pancreatic venous stump draining into the recipient IVC. If a SPK is performed, the kidney graft will then get implanted, often on the recipient left iliac vessels.
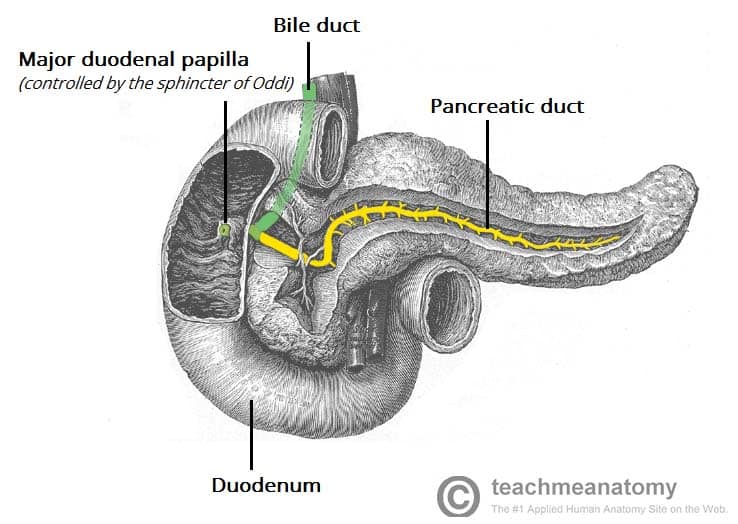
The non-physiological nature of the reconstruction results in insulin by-passing the hepatic first pass metabolism and hence can cause systemic hyperinsulinemia. Pancreatic exocrine drainage is handled by means of anastomosis between the graft duodenum (2nd part) and a small bowel loop, with or without a Roux-en-Y
Complications of Pancreas Transplant
Pancreatic Rejection
Acute rejection occurs in up to 25% of transplants. Diagnosis of rejection in a SPK transplantation is often prompted by raised lipase/amylase and/or hyperglycaemia or increasing HbA1c.
It may be monitored though serum creatinine or blood glucose levels; if in any doubt, a renal or pancreas biopsy can be performed for confirmation although concordant rejection of the kidney only occurs 60-80% of the time, even if from the same donor
Pancreatic Leak
The incidence of pancreatic leaks is around 5-18%. Patients present with abdominal pain, distension, or vomiting, with features of peritonitis on examination if the leak is significant.
Serum amylase levels are raised in 50% of cases. Drain fluid amylase and lipase levels should be checked (very elevated levels suggest a leak) and CT imaging subsequently carried out to assess for abdominal collections.
Conservative management with antibiotics and percutaneous drainage of collections is often sufficient. However, the presence of peritonitis usually requires surgical intervention.
Less commonly, leaks form the enteric anastomosis can occur, usually presenting with sepsis and peritonitis and requiring urgent sepsis management and surgical correction
Vascular Complications
Vascular thrombosis is a very early complication, typically occurring within 48 hours post-operatively. Venous thrombosis in the pancreas portal vein is the most common, presenting with a sudden unexplained return to hyperglycaemia. Thrombectomy can be attempted, although salvage is very uncommon at this stage.
Other complications such as pseudoaneurysms and arterial stenosis can be very difficult to manage without risking graft loss.
Allograft Pancreatitis
Pancreatitis of the allograft occurs to some degree in all patients post-operatively, as part of the ischaemia-reperfusion injury. Patients will present with abdominal pain, tenderness over the graft, fever, or vomiting and is usually self-limiting. More serious cases may contribute to graft loss.
Pancreatitis can also occur because of the development of peri-pancreatic collections, pancreatic leak, or rejection. Management is usually with bowel rest, hydration, and to investigating and treat the cause
Diagnosis is through the hallmark rise in amylase and inflammatory markers, with imaging useful in confirming the diagnosis, as well as ruling out collections or vascular causes. Treatment is usually conservative.
Key Points
- Pancreas transplantation is indicated for the treatment of patients with complicated diabetes mellitus, acting to restore glycaemic control and reduce the impact of diabetes-related complications in certain patients
- Most patients will undergo a simultaneous pancreas kidney transplant (SPK)
- The native pancreas is not removed, with the transplanted graft placed in the lower retroperitoneum
- Complications include graft rejection, leak, thrombosis, or pancreatitis