Introduction
Chronic limb ischaemia is a form of peripheral arterial disease that results in a symptomatic reduced blood supply to the limbs.
It is typically caused by atherosclerosis (rarely vasculitis) and will commonly affect the lower limbs (however the upper limbs and gluteals can also be affected).
Around 15-20% individuals over 70yrs have peripheral arterial disease, although the majority are asymptomatic. The Framingham study demonstrated an increase in the prevalence of the disease from 0.4 per 1000 males aged 35-45yrs to 6 per 1000 males aged >65yrs.
In this article, we shall look at the clinical features, investigations and management of chronic limb ischaemia.
Risk Factors
The main risk factors for chronic limb ischaemia are smoking, diabetes mellitus, hypertension, hyperlipidaemia, increasing age, a strong family history, and obesity or physical inactivity
Clinical Features
The clinical features of chronic limb ischaemia depend on its severity (Table 1)
One of the earlier symptoms is intermittent claudication, a cramping-type pain in the calf, thigh, or buttock after walking a fixed distance (the ‘claudication distance’), that is relieved by rest within minutes. As the disease progresses, the pain becomes constant, even at rest, termed Critical Limb Threatening Ischaemia.
| Stage I | Asymptomatic |
| Stage II | Intermittent claudication |
| Stage III | Ischaemic rest pain |
| Stage IV | Ulceration or gangrene, or both |
Table 1 – Fontaine classification of chronic leg ischaemia
On examination, affected limbs will often be colder than unaffected limbs. There may be evidence of arterial ulcers present, especially in advanced cases, and patients will typically have reduced or absent peripheral pulses.
Buerger’s test involves lying the patient supine and raising their legs until they go pale and then lowering them until the colour returns (or even becoming hyperaemic). The angle at which the limb goes pale is termed Buerger’s angle; an angle of less than 20 degrees indicates severe ischaemia.
Leriche Syndrome
Leriche syndrome is a form of peripheral arterial disease affecting the aortic bifurcation. It specifically presents with buttock or thigh pain and is associated erectile dysfunction.
Critical Limb Threatening Ischaemia
Critical Limb Threatening Ischaemia is the advanced form of chronic limb ischaemia.
It can be clinically defined in three ways:
- Ischaemic rest pain for greater than 2 weeks duration, requiring opiate analgesia
- Presence of ischaemic lesions or gangrene objectively attributable to the arterial occlusive disease (Fig. 1)
- ABPI less than 0.5
On examination, the limbs may be pale and cold, with weak or absent pulses. Other signs include limb hair loss, skin changes (atrophic skin, ulceration, or gangrene), and thickened nails.

Figure 1 – Gangrene as a result of peripheral vascular disease, indicating critical limb threatening ischaemia
Differential Diagnoses
There are two major differential diagnoses* for a patient presenting with limb ischaemia symptoms:
- Spinal stenosis (‘neurogenic claudication’)
- Typically have pain from the back radiating down the lateral aspect of the leg (tensor fascia lata), often have symptoms on initial movement or symptoms that are relieved by sitting rather than standing
- Acute limb ischaemia
- Clinical features that are less than 14 days duration, often presenting within hours.
Other rare causes of non-atherosclerotic lower limb ischaemia include popliteal artery entrapment syndrome, persistent sciatic artery, iliac endofibrosis, cystic adventitial disease, or Buerger’s disease.
*Acute-on-chronic ischaemia is a more complex condition whereby there is an acute often embolic event in a patient with previous peripheral arterial disease. These patients are sub-classified as they typically have a longer duration in which the limb is salvageable.
Investigations
The diagnosis of chronic limb ischaemia is clinical. The ankle-brachial pressure index (ABPI) is used to confirm the diagnosis and quantify severity of chronic limb ischaemia (Table 2); important to remember that any ABPI value >1.2 should be interpreted with caution, as calcification and hardening of the arteries may cause a falsely high ABPI.
| Severity | ABPI |
| Normal | >0.9 |
| Mild | 0.8-0.9 |
| Moderate | 0.5-0.8 |
| Severe | <0.5 |
Table 2 – Severity and ABPI measurement
Any critical limb threatening ischaemia (in the presence of a femoral pulse) should have initial radiological assessment with a Doppler ultrasound, used to assess the severity and anatomical location of any occlusion. Further imaging can be achieved via CT angiography (CTA) or MR angiography (MRA).
Due to concurrent cardiovascular risk factors seen in patients with chronic limb threatening ischaemia, patients should also have a cardiovascular risk assessment. This includes blood pressure, blood glucose, lipid profile and ECG.
Any patient presenting with chronic limb threatening ischaemia <50yrs without significant risk factors should also have a thrombophilia screen and homocysteine levels* checked, and one should think about the non-atherosclerotic lower limb ischaemias listed above.
*A lower homocysteine level has been associated with reduced risk of cardiovascular events
Management
Medical Management
Most patients with chronic limb ischaemia require cardiovascular risk factor modification:
- Lifestyle advice (smoking cessation, regular exercise, weight reduction)
- Statin therapy (ideally atorvastatin 80mg OD)
- Anti-platelet therapy (ideally clopidogrel 75mg OD)
- Optimise diabetes control
Enrollment into a local supervised exercise programme has been shown to improve walking distance and claudication distance, and should be used as first line therapy in any patient without critical limb ischaemia
The course of chronic limb ischaemia is variable and most patients’ symptoms do improve on lifestyle changes and medical management alone. It is important to encourage patients to walk through the pain to encourage the development of new blood vessels and establishment of a collateral circulation.
Surgical Management
Current guidance states that surgical intervention can be offered in suitable patients if (i) risk factor modification has been discussed; and (ii) supervised exercise has failed to improve symptoms. This should be discussed based on the walking distance of the patient, and risks of surgery.
Any patients with critical limb ischaemia should be urgently referred for surgical intervention. Patients who are an inpatient should be treated within 5 days; if they are stable, and if suitable for an outpatient pathway, they should be treated within 2 weeks.
There are two main surgical options available:
- Angioplasty with or without stenting (Fig. 2)
- Bypass grafting, typically used for diffuse disease or in younger patients
A combination, such as initial surgery to clean a specific lesion allowing access for angioplasty to another region, can often be trialled, for example the common femoral artery is often used as a vascular access site, however if occluded then common femoral endarterectomy is required and the patient can then have a stent or bypass from that location.
Amputations are considered for any patients who are unsuitable for revascularisation, with ischaemia causing incurable symptoms or gangrene leading to sepsis.
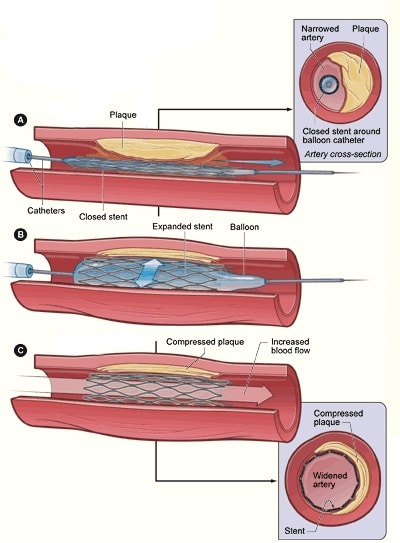
Figure 2 – Schematic demonstrating angioplasty and stenting for patients with limb ischaemia
Complications
Chronic limb ischaemia can result in sepsis (secondary to infected gangrene), acute-on-chronic ischaemia, amputation, and reduced mobility and quality of life.
Over a 5 year period, of those patients with intermittent claudication:
- Most will have stable claudication or improve
- 10-20% develop worsening symptoms
- 5-10% develop critical limb ischaemia
Two years following a below-knee amputation for chronic limb ischaemia, 15% require a further above knee amputation, 30% have died, and only 40% have full mobility.
The 5 year mortality rate in those diagnosed with chronic limb ischaemia is around 50%. Amputation is eventually required in 1-2% of all cases (increases to 5% in people with diabetes mellitus)
Key Points
- Chronic limb ischaemia is a common condition, ranging in severity across the population, associated with several cardiovascular risk factors
- Whilst a clinical diagnosis, it can be quantified by ABPI testing, following by imaging
- Surgical intervention can be offered if conservative management options fail or for those presenting with critical limb threatening ischaemia
- The 5 year mortality rate in those diagnosed with chronic limb ischaemia is around 50%
