Introduction
Thoracic outlet syndrome (TOS) refers to the clinical features that arise from compression of the neurovascular bundle within the thoracic outlet.
The signs and symptoms that arise can be divided into neurological (nTOS, most common), venous (vTOS), and arterial (aTOS). Most people affected are between 20-50 years old.
It usually occurs in the setting of hyperextension injuries, repetitive stress injuries (e.g. work-related, particularly when working over the head), or external compressing factors (e.g. poor posture), but can also be secondary to anatomical abnormalities, including that of the 1st rib, an anomalous cervical rib, or bands within the thoracic outlet.
Pathophysiology
The brachial plexus and subclavian artery pass through the scalene triangle, and the subclavian vein passes anterior to anterior scalene. The brachial plexus can be compressed between the anterior and middle scalene muscles, or against the 1st rib or a cervical rib; typically, it is the lower cord which becomes irritated (resulting in symptoms affecting the ulnar distribution).
As such, hypertrophy of the scalene muscles, abnormality in the first rib, or the presence of a cervical rib can all lead to compression on the brachial plexus or subclavian artery. Previous clavicle fracture can cause abnormal bony healing that compresses on the thoracic outlet. The presence of a costoclavicular ligament can reduce the costoclavicular space, leading to vTOS, due to positional venous obstruction.
Cervical Rib
A cervical rib is an extra rib that arises from the seventh cervical vertebra (Fig. 2). It occurs in 0.2-0.5% of the population and can be partial or complete.
Whilst this increases the risk of thoracic outlet syndrome, the majority of patients with a cervical rib are unaware of it and causes no symptoms. Identification of a cervical rib in an otherwise asymptomatic patient does not warrant any intervention.
Risk Factors
Recent trauma, repetitive motion occupations, athletes*, or anatomical variations are potential risk factors for TOS
*It is more common in athletes that use repetitive arm motions, such as swimming and racquet sports, and in bodybuilders
Clinical Features
The specific clinical features present will be dependent on neurological, arterial, or venous involvement. Symptoms may also worsen with certain movements, e.g. shoulder abduction or extension.
- Compression of the brachial plexus can cause paraesthesia and/or motor weakness, which is often in the ulnar distribution; there may be muscle wasting, and pain can radiate to the neck and upper part of the back
- Venous compression can lead to deep vein thrombosis and extremity swelling (termed Paget-Schrötter syndrome); in untreated severe cases, there can be prominent veins over the shoulder due to collateralisation
- Arterial compression can cause claudication symptoms or acute limb ischaemia through either occlusion, distal embolisation, or aneurysm formation
On examination, assess for areas of weakness or numbness, for swelling or tenderness, and any features of limb ischaemia. Tenderness over the scalene muscles is often present.
Special Tests for Thoracic Outlet Syndrome
- Adson’s manoeuvre – Palpate the radial pulse on the affected side, with the arm initially abducted to 30 degrees, then ask the patient to turn their head and look at the affected side’s shoulder; fully abduct, extend, and laterally rotate the shoulder
- Any decrease or loss of pulse is suggestive of TOS
- Roo’s test – Abduct and externally rotate the shoulder on the affected side to 90 degrees, bend the elbow to 90 degrees, then ask the patient to open and close the hands slowly over a 3-minute period
- Any worsening of symptoms will develop if TOS is present
- Elvey’s test – Extend the arm to 90 degrees, with the elbow extended and wrist dorsiflexed, then tilt the patients ear to each shoulder
- Any loss of the radial pulse or worsening symptoms is suggestive of TOS
Investigations
Initial blood tests should be taken, including FBC and clotting screen (further specialist haematological testing may be warranted later for further assessment).
A chest radiograph (CXR) is important to identify potential bony abnormalities* such as cervical ribs (Fig. 2), long transverse cervical processes, or rib/clavicular fracture calluses
*Over 90% of aTOS patients will have a bony abnormality
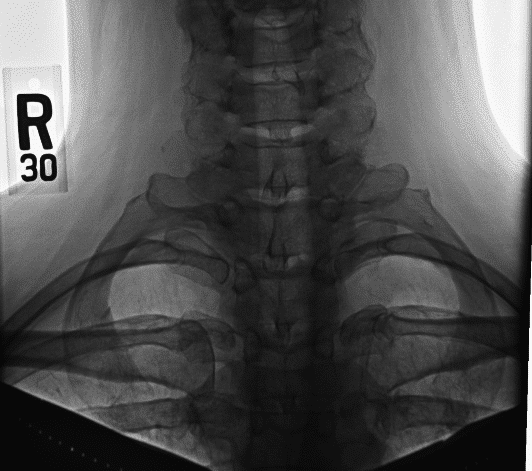
Figure 2 – Bilateral cervical ribs, as seen on chest radiograph
Further Investigations
For suspected venous or arterial TOS, common tests used for diagnosis include initially a venous and arterial duplex ultrasound study, particularly with the patient at rest and with the arm in stress positions to look for any compression. CT or MRI imaging or a venogram may be required for further assessment.
For neurogenic cases, nerve conduction studies are a common investigation, as they allow detection of decreased action potential conductance because of nerve compression. Typically, they are used to rule out carpal tunnel and cubital tunnel syndrome, rather than diagnose nTOS.
MRI imaging can be used for detection of cervical ribs and fibrous bands, if suspected. Any patient presenting with acute limb ischaemia secondary to aTOS needs an urgent CT angiogram arranged.
Management
The treatment approach depends upon the type of TOS
For nTOS, the first line management is physiotherapy, over the course of around 6 months, aiming to improve mobility in the neck and shoulder, strengthen the surrounding muscles, and relax the scalene muscles. Botulinum toxin injections can also be effective to help relax the scalene muscles, often done concurrently to aid physiotherapy.
Patients with vTOS may need thrombolysis and anti-coagulation, under guidance form the haematology teams, however most cases will need surgical management to decompress the thoracic outlet, as well as venoplasty or venous reconstruction or the placement of a venous stent.
For aTOS with acute limb ischaemia, urgent vascular input is required, as the patient may warrant an embolectomy. However, most cases are causes by anatomical abnormalities that can be managed in the elective surgical setting.
Surgical Management
Surgical procedures should be considered if conservative measures do not work or anatomical variations require correction (required in around 10% of cases). Elective surgery in aTOS or vTOS typically corrects symptoms in 90-95% of cases, but only in 50-70% in nTOS.
For decompression procedures, this can either be via a supraclavicular or transaxillary approach, allowing access to excise the first or cervical rib. Any restrictive bands can be released too (or even the anterior scalene muscle), if also impinging on surrounding structures.
Complications of TOS surgery include the neurological or vascular damage, or haemothorax, pneumothorax, or chylothorax (particular on the left, the thoracic duct is within the thoracic outlet can is at risk of damage).
Complications
Left untreated, TOS can lead to further sequelae of the pathology, including permanent nerve damage, aneurysmal dilation of the subclavian artery leading to embolisation, or loss of limb function.
Prognosis in neurological TOS is variable, whilst that of vascular TOS is largely favourable after appropriate surgical intervention.
In some cases, especially nTOS, symptoms can persist despite aggressive physiotherapy and surgical intervention. Symptoms can recur from 1 month to 10 years after surgical intervention.
Key Points
- Thoracic outlet syndrome refers to the clinical features that arise from compression of the neurovascular bundle within the thoracic outlet
- Commonly occurs due to hyperextension injuries, repetitive stress injuries, or anatomical abnormalities
- Patients present with either neurological (most common), venous, or arterial sequelae clinical features
- Investigation and management is dependent on the underlying cause and subtype of thoracic outlet syndrome

