Introduction
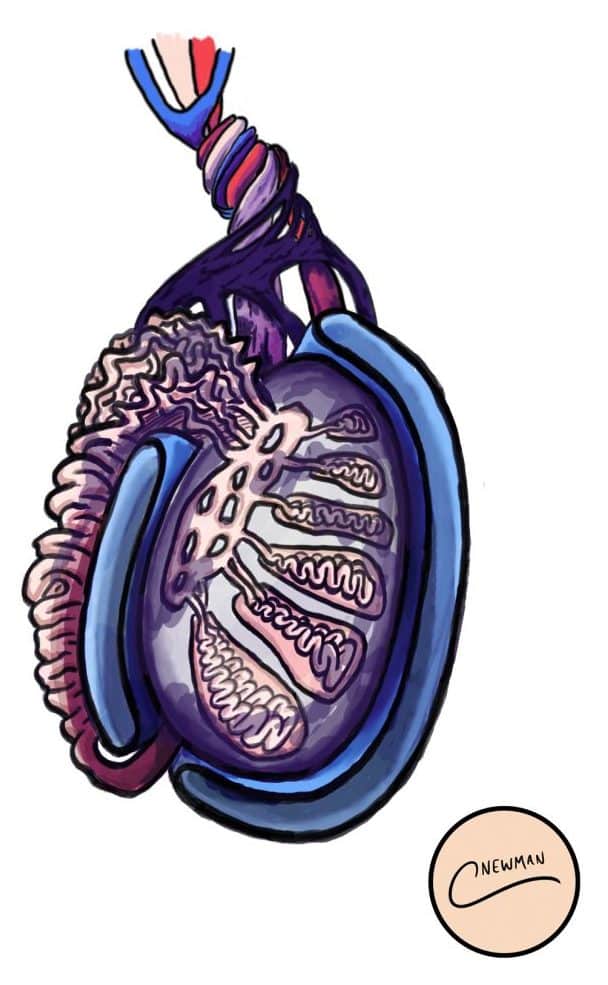
Testicular torsion occurs when the spermatic cord and its contents twists within the tunica vaginalis, compromising the blood supply to the testicle.
Testicular torsion is a surgical emergency, as without treatment the affected testicle will infarct and die within hours. Whilst theoretically it can occur at any age, peak incidence is in neonates and adolescents between the ages of 12-25yrs.
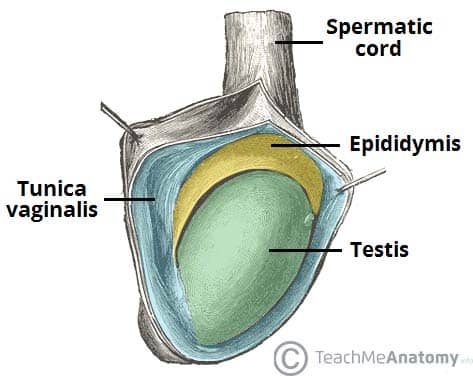
Figure 1 – The testes and epididymis, surrounded by the tunica vaginalis
Pathophysiology
Torsion occurs when a mobile testis rotates on the spermatic cord. Initially, this blocks venous return as the veins are thin walled, causing venous congestion and subsequent oedema. As congestion worsens, rising pressure then restricts arterial blood flow, cutting off oxygen supply and leading to ischemic injury.
Males with a horizontal lie to their testes, often termed a ‘bell-clapper deformity’, are more prone to developing testicular torsion. In this anatomical variant, the testis lacks normal attachment of the tunica vaginalis and often the gubernaculum, making it more mobile and significantly increasing the likelihood of twisting on the cord structures.
Neonatal Testicular Torsion
In neonates the attachment between the scrotum and tunica vaginalis is not fully formed and the entire testis and tunica vaginalis can tort; this is known as ‘extra-vaginal torsion’.
It is important to note that this can occur in-utero and new-borns must be thoroughly examined at their first check. Almost all other torsions will be ‘intra-vaginal’, with the freely moving cord and testis torting within the tunica vaginalis.
Risk Factors
The main risk factors for developing a torsion are:
- Age (most common 12-25yrs)
- Previous testicular torsion*
- Family history of testicular torsion
- Undescended testes
*Previous non-specific episodes of testicular pain that have self-resolved could be a sign of previous torsion with self-detorsion (often termed torsion-detorsion syndrome)
Clinical Features
Patients will generally present with sudden onset severe unilateral testicular pain. This is often associated with nausea and vomiting, secondary to the pain. Referred abdominal pain can also occur.
On examination, the testis will have a high position* (compared to the contralateral side) with a horizontal lie. It can also appear swollen and will be extremely tender.
Classically, the cremasteric reflex is absent and pain continues despite elevation of the testicle, termed a negative Prehn’s sign (whilst in epididymo-orchitis, Prehn’s test is often positive).
*It is often worth clarifying with the patient the normal position of their testes in their scrotum (i.e. which testis normally sits higher)
The TWIST Score
The TWIST score (Testicular Workup for Ischemia and Suspected Torsion) is increasingly being used to differentiate between patients who require immediate scrotal exploration versus those who may benefit from ultrasonography.
This clinical tool assesses the likelihood of testicular torsion in individuals presenting with acute scrotal pain by evaluating five key signs: testicular swelling (2 points), hard testis (2 points), absent cremasteric reflex (1 point), nausea/vomiting (1 point), and high-riding testis (1 point).
A score of 0-2 indicates a low risk, 3-4 suggests moderate risk, and a score of 5-7 strongly indicates torsion, necessitating immediate surgery without additional imaging.
Differential Diagnosis
The most common differential to exclude is epididymo-orchitis; this is normally associated with a more gradual onset of pain and can be associated with LUTS and / or pyrexia.
Other differentials to consider include trauma, incarcerated inguinal hernia, testicular cancer, renal stones, hydrocele, idiopathic scrotal oedema, and torsion of the hydatid of Morgagni (see below).
Torsion of the Hydatid of Morgagni
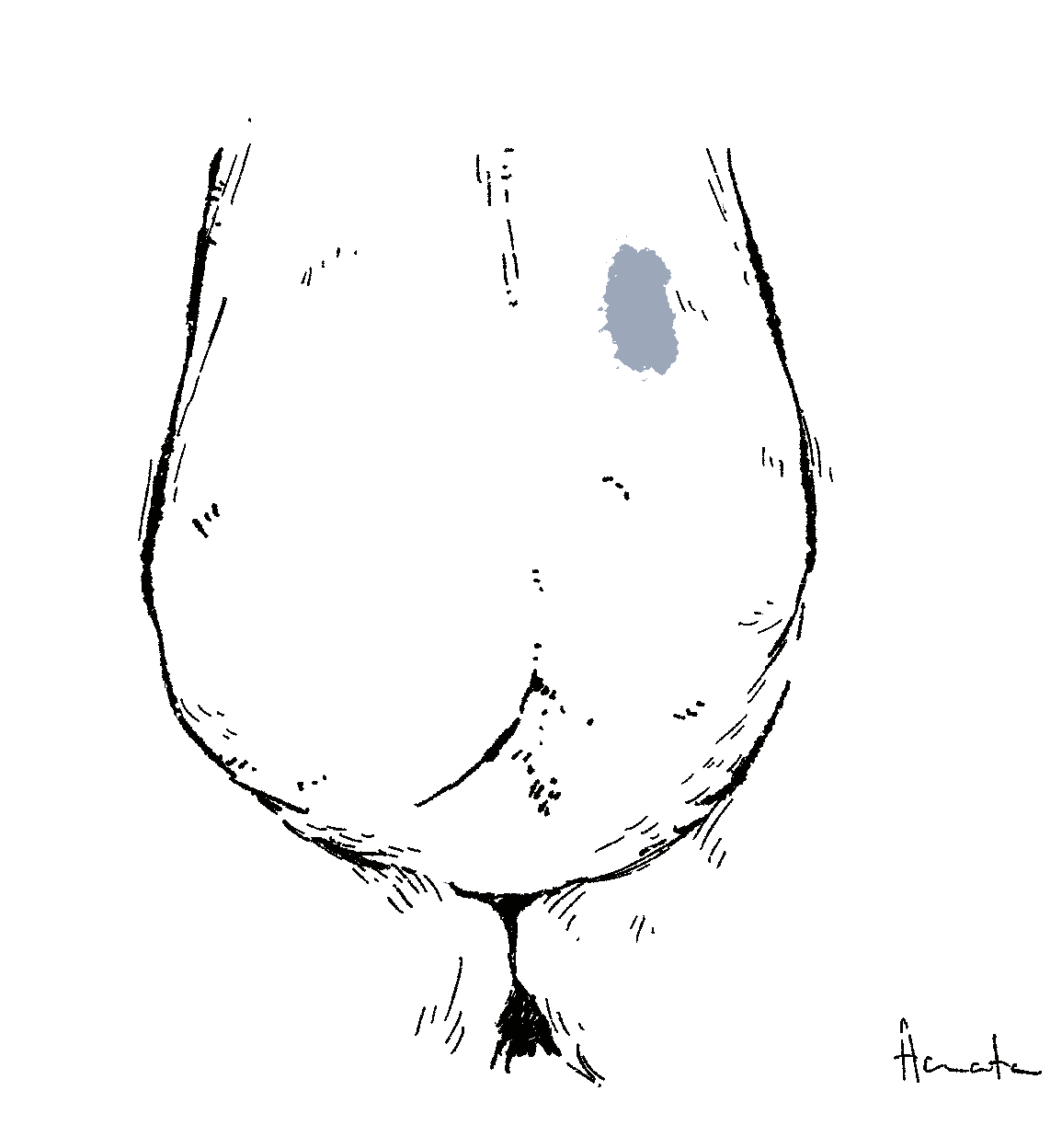
The hydatid of Morgagni is a remnant of the Mullerian duct and is a common testicular appendage. This structure can also become torted, presenting with similar sudden onset pain.
Torsion of these structures is more common in a younger age group than testicular torsion, and the scrotum is usually less erythematous with a normal lie of the testis.
The ‘blue dot’ sign may be present in the upper half of the hemiscrotum, which is the visible infarcted hydatid. It is worth noting that this sign is relatively rare and can be difficult to appreciate in patients with darker skin tones.
Investigations
The diagnosis of testicular torsion is a clinical one, therefore any suspected cases should be taken straight to theatre for scrotal exploration.
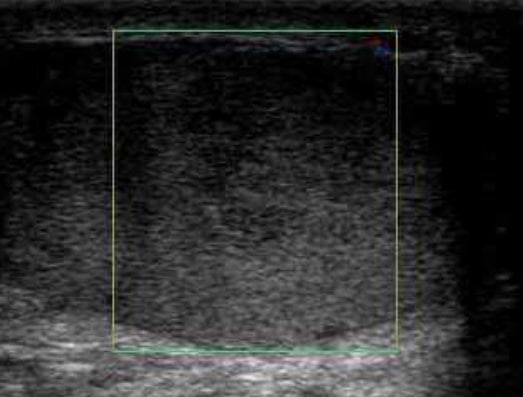
However, in cases with sufficient equipoise, Doppler ultrasound (Fig. 4) can be used to investigate potential compromised blood flow to the testis (if available, this test has a high sensitivity (89%) and specificity (99%)).
A urine dipstick can also be performed to assess for any potential infective component, as part of potential differentials.
Management
Testicular torsion is a surgical emergency with a 4-6hrs window from the onset of symptoms to salvage the testis before significant ischaemic damage occurs.
Any suspected case warrants urgent surgical exploration of the testis to assess the testes and the spermatic cord for evidence of torsion.
Patients should be provided with suitable strong analgesia and anti-emetics pre-operatively, and made nil by mouth with maintenance fluids prescribed.
Surgical Management
If torsion is confirmed intra-operatively, the cord and testis will be untwisted and both testicles fixed to the scrotum, termed bilateral orchidopexy (prevent further any further torsion episodes)*.
In cases where the testis is non-viable, an orchidectomy may be warranted; prosthesis can be inserted at time of surgery or at a later date, at the patient request.
*It recommends that if no torsion is identified during exploration, the testis should not be fixed, and the contralateral testis should also remain unexplored and unfixed unless a bell clapper deformity is detected on the symptomatic side
Complications
Delay in surgical exploration leading to prolonged ischaemia can result in testicular infarction; the chance of this happening increases exponentially with time since onset of pain*.
Despite expedient scrotal exploration, de-torsion, and orchidopexy, the affected testis may later undergo atrophy. Patients undergoing scrotal exploration should be consented for chronic pain, palpable suture, risk to future fertility, and a theoretical risk of future torsion despite fixation.
*Testicular salvage rates are 90-100% if surgery performed within 6hrs of onset of pain, and this decreases to 50% if symptoms are present for more than 12 hours
Key Points
- Testicular torsion is a surgical emergency
- It presents with sudden onset severe unilateral testicular pain
- Suspected cases warrant urgent surgical exploration
- Confirmed cases intra-operatively will require bilateral orchidopexy