Hyperkalaemia is defined as an elevated serum potassium, greater than 5.5 mmol/l (may vary depending on local reference ranges)
Whilst usually asymptomatic at relatively low levels, it is important to identify and treat the condition early due to cardiac and other complications that may arise.
Causes
The most common causes of hyperkalaemia in the post-operative patient are:
- Post-operative Acute Kidney Injury
- Repeated blood transfusions
- Drugs:
- Potassium-Sparing Diuretics, including Spironolactone
- ACE inhibitors (or ARBs)
- Excessive potassium treatment
Presentation
A patient may commonly be asymptomatic; symptoms are rare in patients with a potassium serum concentration of less than 7.0mmol/l.
Any symptoms of hyperkalaemia that may present include paraesthesia, muscle weakness, nausea and vomiting, and palpitations.
Assessment and Investigations
The assessment of any patient with hyperkalaemia needs to be timely and is often performed simultaneously with treatment. The initial investigations required are:
- Routine bloods, including U&Es, Ca2+ and PO42-, and Mg2+
- Venous blood gas (VBG)
- A VBG will provide an immediate result of the patient’s potassium levels
- ECG (as discussed below)
- Catheterisation, if necessary (for fluid balance monitoring)
The patients observations and fluid status should be reviewed, as well as their medication (identifying any precipitants of hyperkalaemia).
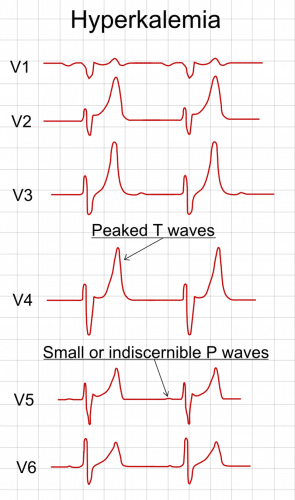
ECG Changes in Hyperkalaemia
The ECG is vital in the assessment of hyperkalaemia, as ECG findings will progress with increasing serum levels.
Whilst the ECG findings generally can be correlated to the serum potassium concentration (Fig. 1), potentially life-threatening arrhythmias can occur without warning in hyperkalaemia.
- Mild (5.5 – 6.5mmol)
- Tall ‘tented’ T waves (seen across the precordial leads)
Prolonged PR segment
- Tall ‘tented’ T waves (seen across the precordial leads)
- Moderate (6.5 – 7.5mmol)
- Decreased or ‘flattened’ P wave
Prolonged QRS complex
- Decreased or ‘flattened’ P wave
- Severe (> 7.5mmol)
- Progressive widening of the QRS complex
Axial deviation and Bundle Branch Blocks
- Progressive widening of the QRS complex
The progressively widened QRS eventually merges with the T wave, forming a sine wave pattern. Subsequent Ventricular Fibrillation (VF) or asystole may then follow.
Management
The management of a hyperkalaemic patient can be considered in three parts:
- Stabilisation of the myocardium
- Reduction of serum potassium
- Reduction of total body potassium
Whilst the rationale for the first and second management strategies may be self-evident, it is important to consider that the underlying cause for the hyperkalaemia must also be addressed.
Early and repeated blood testing is vital and any ECG changes warrant urgent treatment and moving the patient to a high-dependency area. Alert a senior to any complications developing.
Stabilisation of the Myocardium
A stat dose of intravenous Calcium Gluconate or Calcium Chloride (typically 10ml of 10%, dependent on local guidelines) should be started, either when ECG changes are present or in all cases of moderate or severe hyperkalaemia
Continuous cardiac monitoring is required following stabilisation treatment in such cases.
Reduction of Serum Potassium
Variable rate insulin with dextrose infusion should be started (typically 200ml of 20% glucose with 10U of insulin over 30mins, yet varies with local policy), acting to increase cellular uptake of potassium and thus reduce serum concentration.
These measures are only short term, as the potassium will leave the cells within 30-60 minutes, therefore repeated doses may be required. Salbutamol nebulisers may also be additionally added in for further (albeit limited) reduction.
Reduction of Total Body Potassium
Any reversible underlying cause should be identified and appropriately managed*.
Referral to renal physicians may be warranted in cases of severe hyperkalaemia or resistant hyperkalaemia potentially warranting haemodialysis.
*Oral calcium resonium can be used to reduce total body potassium, reabsorbing potassium into the bowel intra-luminally, however this step is complex and specialist input should be sought early.
Key Points
- Hyperkalaemia is an elevated serum potassium
- There are several potential causes of hyperkalaemia, most commonly renal impairment or iatrogenic
- Typically asymptomatic, however can cause cardiac instability if not identified and treated appropriately
- Management involves stabilisation of the myocardium, reduction of serum potassium, and reduction of total body potassium