Introduction
Patella fractures account for approximately 1% of all skeletal injuries and are most prevalent in 20-50 year olds. They are twice as common in males.
They typically occur as a result of direct trauma to the patella, however less commonly can occur as a result of rapid eccentric contraction of the quadriceps muscle.
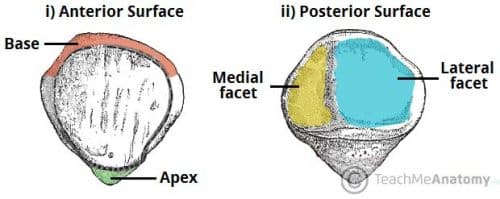
The patella itself is the largest sesamoid bone in the body, formed within the tendon of the quadriceps femoris muscle as it crosses over the anterior aspect of the knee joint, attaching to the patellar ligament inferiorly. Its posterior surface consists of medial and lateral facets that articulate with their respective femoral condyles (Fig. 1).
Clinical Features
Patients will present with anterior knee pain, following a mechanism of injury such as a hard blow to the patella (e.g. dashboard injury in a RTA) or strong contraction of the quadriceps.
The pain will be made worse with movement and the patient will be unable to straight leg raise (due to damage to the extensor mechanism). They may not be able to weight bear.
On examination, the affected knee will be significantly swollen and bruised. Often a visible and palpable patellar defect is present between the bone fragments.
Differential Diagnosis
Differentials for a patient presenting with knee pain following trauma may have a tibial plateau fracture, distal femur fracture, or cruciate or collateral ligament injury. The differentials for knee pain following sudden extension of the knee include quadriceps tendon rupture.
Bipartite Patella
Bipartite patella is a congenital condition affecting 2-3% of the population (more common in males), whereby there is failure of patella fusion, leaving two separate bone fragments of the patella joined only by fibrocartilaginous tissue.
The condition is typically asymptomatic and usually only picked up incidentally on imaging. Rarely, bipartite patella can present symptomatically, especially after exercise or overuse, with anterior knee pain.
Investigations
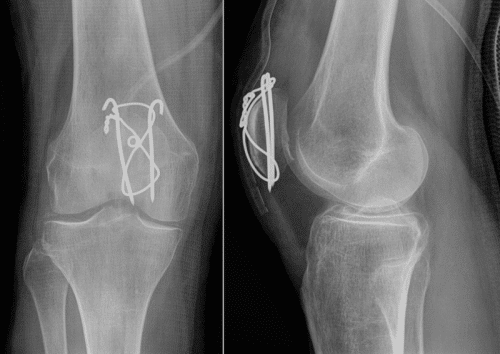
The mainstay of investigation for suspected patella fracture is plain film radiographs (Fig. 2), obtaining three separate views (antero-posterior, lateral, and skyline*)
More advanced imaging (usually CT) is indicated in comminuted fractures or in cases not overtly apparent on plain films but clinically suggestive.
*Skyline view is often not possible in actual cases of patella fracture due to pain inhibiting knee flexion to the necessary 30 degrees
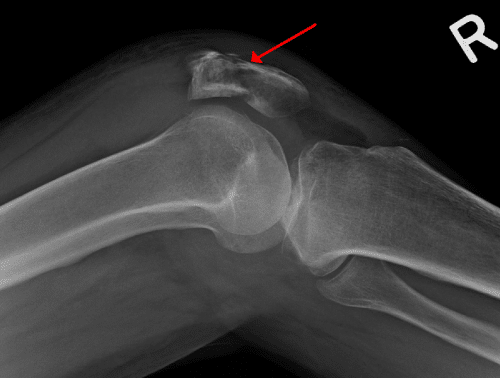
Figure 2 – Lateral view plain film radiograph of a patella fracture
The AO Foundation Classification classifies patella fractures into three groups (1) extra-articular or avulsion fractures (2) partial articular fractures (3) complete articular fractures.
Management
Conservative management is often used in cases of non-displaced or minimally displaced patella fractures, or with vertical fractures providing that the extensor mechanism remains functional.
Patients are placed in a brace or cylinder cast, ensuring early weight bearing in extension with initial minimal displacement and articular step-off, before increasing flexion incrementally.
Surgical Management
Operative intervention is indicated in cases of significant displacement or compromise to the extensor mechanism. The aim of surgery is to obtain anatomical reduction, adequate fixation, and restoration of the extensor mechanism.
Open reduction and internal fixation (ORIF) with tension band wiring is the most widely accepted method (Fig. 3). This aims to convert the tensile force applied to the patella via the extensor mechanism into a compression force to assist with fracture reduction and healing.
In cases of simple vertical or transverse fractures occurring in the context of healthy cancellous bone, screw fixation can be used without the use of wires. In rare cases when ORIF is not possible, partial or total patellectomy may be considered.
Complications
Loss of range of motion in the knee is the primary complication of patella fractures affecting both conservative and operatively managed patients. Patients are also at a risk of secondary osteoarthritis (at the patellofemoral joint) following a patella fracture.
Key Points
- Patella fractures typically occur following direct trauma to the patella
- Patients will present with severe knee pain and an inability to straight leg raise
- Suspected patella fracture require plain film radiographs, in antero-posterior, lateral, and skyline views
- Management is operative in severely displaced cases or those with loss of extensor mechanism, often using tension band wires