Introduction
A pseudoaneurysm, also known as a “false aneurysm”, occurs when there is a breach to the arterial wall, resulting in an accumulation of blood between the tunica media and tunica adventitia of the artery.
There is a direct communication between the vessel lumen and aneurysm lumen, meaning the size of the pseudoaneurysm can continue to increase. Small pseudoaneurysms may be managed conservatively and thrombose, however many will continue to grow until, if left untreated, they perforate.
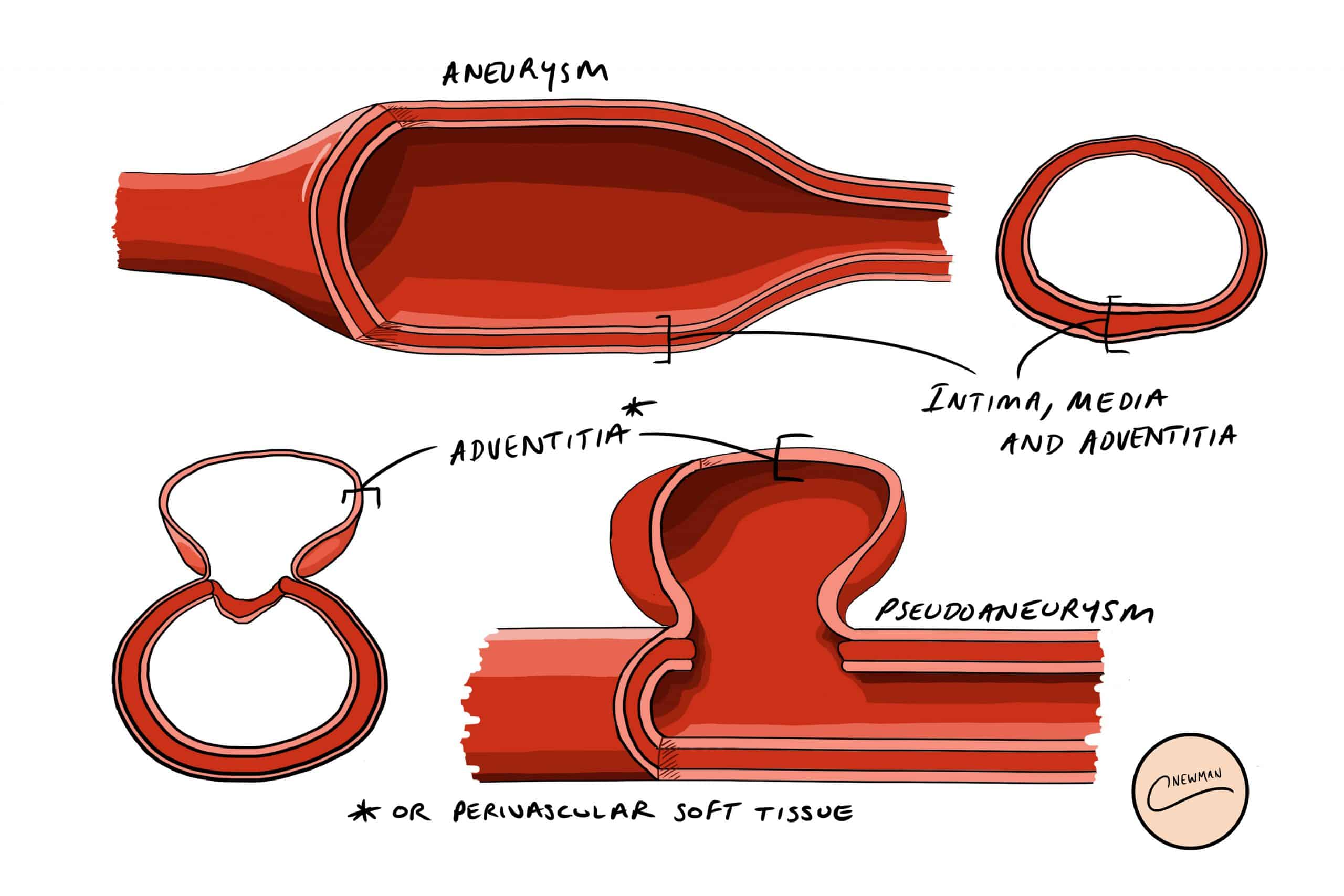
Figure 1 – Layers of the arterial wall involved in an aneurysm and in a pseudoaneurysm
They typically occur following damage to the vessel wall, such as puncture following cardiac catheterisation or repeated injections to the vessel (e.g. from intravenous drug use (IVDU)); other causes include trauma, regional inflammation*, or vasculitis. They are most common at the femoral artery, but can also occur at the radial artery, carotid artery, or abdominal/thoracic aorta.
If a pseudoaneurysm becomes infected, which is more common in IVDU patients (from introduction of pathogens through non-sterile needles), then patients can quickly become septic and the pseudoaneurysm becomes even more likely to rupture.
*Splenic artery pseudoaneurysm formation is a known complication of acute pancreatitis
Aneurysms Versus Pseudoaneurysms
An aneurysm is an abnormal dilation of an artery that involves all three layers of the arterial wall (intima, media and adventitia), whilst a pseudoaneurysm is a collection of blood between the media and adventitia layers
Aneurysms are caused by dilatation of all layers of the arterial wall, and are more common in males, smokers, patients with a family history, and with increasing age, whilst pseudoaneurysms are typically caused by direct trauma to the vessel.
Clinical Features
Patients typically present with a pulsatile lump, which can be tender and painful. The most common location of a pseudo-aneurysm is the femoral artery, however, in theory, they can present in any arterial location. There may be distal arterial occlusion due to compression from the pseudoaneurysm, leading to limb ischaemia, therefore ensure to check distal pulse status.
If infected, the area will be erythematous and tender; purulent material may be discharging from any sinus opening present. The patient will likely have systemic features of sepsis, including pyrexia and tachycardia.
Any patient that reports they had bleeding from the pseudoaneurysm that has since stopped requires close monitoring and urgent management, as this may represent a “herald bleed” that could rebleed at any time.
Differential Diagnosis
The main differentials for pseudoaneurysms include true aneurysms, haematomas (especially after a procedure or trauma), or abscess (especially in an IVDU).
Investigation
Due to the similar presentations that the differentials present with, imaging is required to confirm the diagnosis. It is however imperative that distal pulse status is assessed (and documented) prior to any intervention.
The gold-standard is with duplex ultrasound, which will show turbulent forward and backward flow (termed “yin-yang sign”). CT imaging can be used if access is difficult with ultrasound, which will delineate any smooth walled sac adjacent to the artery.
For any infected pseudo-aneurysm, ensure that routine bloods (FBC, CRP, U&Es, clotting) are sent, as well as blood cultures and a pus MC&S (if discharging). Due to their high risk of rupture, ensure sufficient blood units are cross-matched.
Management
Whilst small pseudoaneurysms can be left alone, the management for most larger or symptomatic pseudoaneurysms is through either ultrasound-guided compression or thrombin injection. Compression can be painful to do and requires 30 minutes of direct pressure of the neck of the pseudoaneurysm.
Ultrasound-guided thrombin injection technique involves the injection of thrombin directly into the lumen of the pseudoaneurysm under ultrasound guidance (Fig. 3), to form a thrombus within the pseudoaneurysm and close it off. Success with this technique is highest in pseudoaneurysms with long and narrow necks. The patient can then have follow-up imaging to ensure resolution.
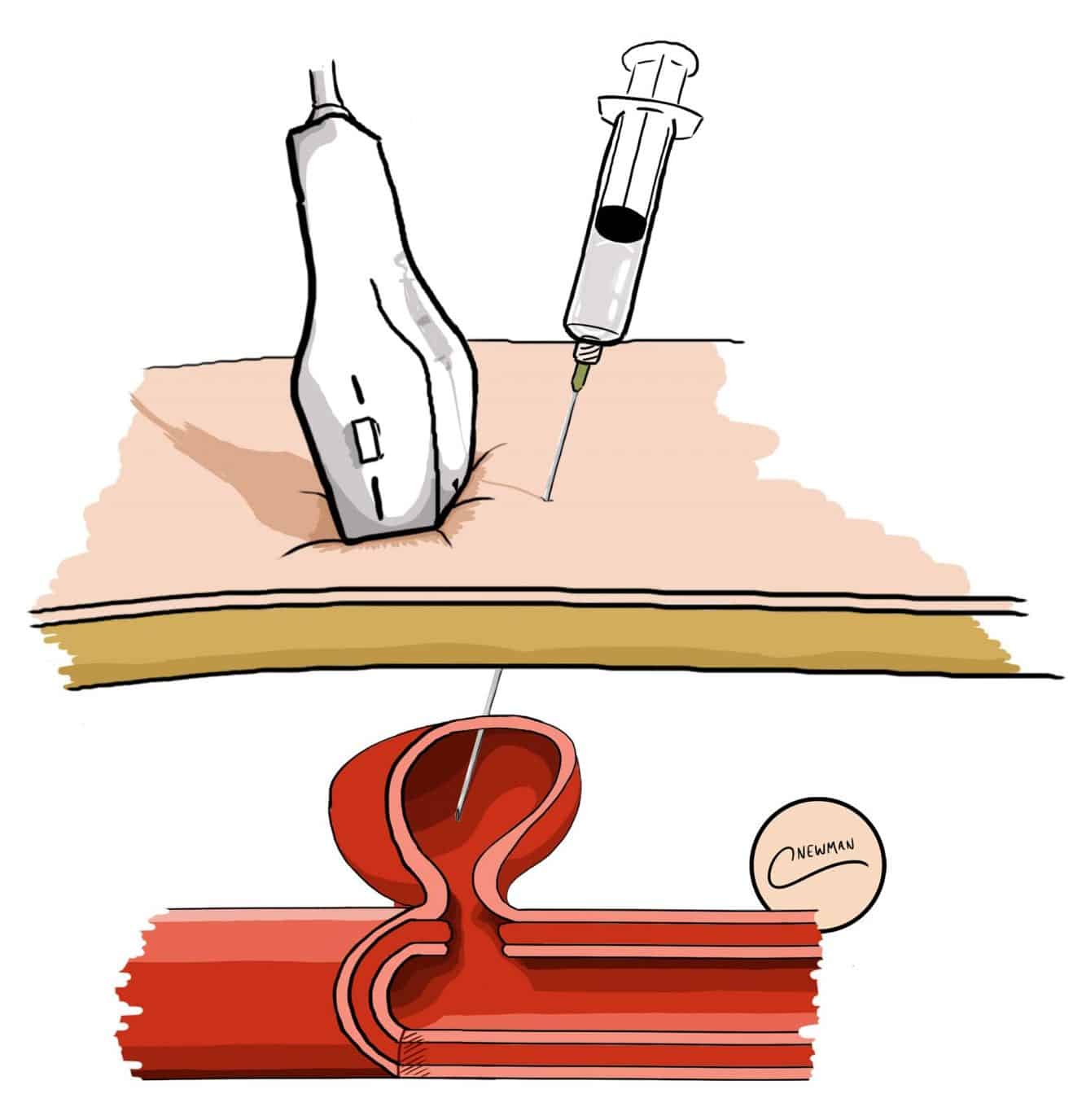
Figure 3 – Illustration of Ultrasound-Guided Thrombin Injection of a Pseudoaneurysm
The options of endovascular stenting or surgery depend upon the patient and the location of the pseudoaneurysm. Endovascular covered stents can be deployed with good success rates, however this is often not possible due to the location of the pseudoaneurysm meaning that there is insufficient space to land a stent without covering a major branch. They can also leak causing persistent perfusion of the pseudoaneurysm, or migrate.
Surgical repair or ligation of the pseudo-aneurysm can be performed. Healthy artery proximal and distal to the pseudoaneurysm should be controlled prior to opening the pseudoaneurysm. It may then be possible to repair the defect in the artery directly, or with a vein or bovine patch; occasionally ligation is required, however this may cause distal ischaemia and require a bypass graft.
Infected Pseudoaneurysms
For infected pseudoaneurysms, their risk of perforation is much higher, which will lead to significant haemorrhage if left untreated. If any evidence of discharge from the region, a pressure dressing should be applied and urgent imaging obtained.
Infected pseudoaneurysms will require surgical ligation. The majority of patients will not develop acute limb ischaemia due to this, however occasionally a bypass graft will be required. Due to this being an infected area any bypass can become infected, and therefore using vein or bovine grafts is preferable as they are more resistance to infection, and tunnelling the graft through a non-infected area is recommended.
Collateral supply following ligation can provide adequate blood flow distally in most cases, however unfortunately (for femoral artery involvement) a small proportion will end up needing subsequent amputations.
Key Points
- A pseudoaneurysm occurs when there is a breach to the arterial wall, resulting in an accumulation of blood between the tunica media and tunica adventitia of the artery
- Patients typically present with a pulsatile lump, which can be tender and painful; the most common site of occurrence is at the femoral artery
- Mainstay of investigation is with a duplex ultrasound
- Small pseudoaneurysms can be left alone, however larger or symptomatic pseudoaneurysms will need either ultrasound-guided compression or thrombin injection
- Infected pseudoaneurysms are more prone to rupture and therefore need urgent investigation and management

