Introduction
The role of cardiopulmonary bypass (CPB) is to take over the function of the heart and lungs, and to deliver oxygen uninterrupted to the vital end organs for the purposes of heart-lung surgery.
The essential functions of CPB are in its ability to provide oxygenation, ventilation, circulation, temperature control, and electrolyte balance during these procedures. The extracorporeal circulation that is involved means that CPB can function as both circulatory support and respiratory support.
CPB and the cardioplegia solution (which is administered once cardiopulmonary bypass is established) provide myocardial protection and decompresses the heart, reducing the energy expenditure during the period of ischaemia that occurs during the procedure.
Pathophysiology
The physiological changes that occur from CPB during the intra- and post-operative periods are as a result of the whole-body inflammatory response secondary to the passage of blood though non-endothelial lined tubes. During the procedure and whilst on CPB, five plasma protein systems are seen to activate; the contact system, the intrinsic and extrinsic coagulation pathways, the complement system, and the fibrinolytic pathway.
The initial contact with the non-endothelial lined tubes activates the contact system; factor XI (which is part of contact system) in turn will activate the intrinsic coagulation pathway, whilst tissue damage during the surgery itself activates the extrinsic coagulation pathway. The complement pathway will be activated by factor XIIa (another component of the contact system), whilst endothelial cells react to circulating thrombin by producing tissue plasminogen activator that activates the fibrinolytic pathway.
Cardinal Effects on Systems
Whilst there are sizeable benefits of CPB, there remain systemic side-effects that occur with its use.
Both a reduced cardiac contractility and increased pulmonary resistance (from protamine-induced pulmonary hypertension) are seen in patients on CPB. Acute respiratory distress syndrome can also occur as a result of the inflammatory responses that occur.
Inflammatory pathway activation in CPB (as described above) can make patients both hypercoagulable and antithrombotic. The impact of the inflammatory response also means these patients can be more susceptibility to infection.
Changes in fluid status, particularly with intravascular depletion, can impact the kidneys during CPB, resulting in acute kidney injury. Gastrointestinal or neurological deficits are less common.
The Circuit
The flow of blood from patient to bypass machine back to patient follows a specific sequence that maximises perfusion and minimises risk (Fig. 3).
The key steps involved in setting up the circuit are:
- Heparisation of the blood, with subsequent insertion of the CPB cannulas (most common route is aorto-atrial); drain the blood from the right atrium into a reservoir, then subsequently drain of the blood from the left ventricle (for decompression, termed myocardial protection) also into a reservoir
- Propel the blood via a pump from the reservoir through a heat and gas exchanger, then through an arterial filter, allowing the blood to enter the patient via the aortic cannula; place an aortic cross clamp, to separate the systemic and coronary circuits and to avoid mixing of circulation solutions
- Propel potassium rich cardioplegia solution through the gas exchanger to the cardioplegia pump, which ensures the cardioplegia solution passes into the aortic root (antegrade cardioplegia) or into the coronary sinus (retrograde cardioplegia)
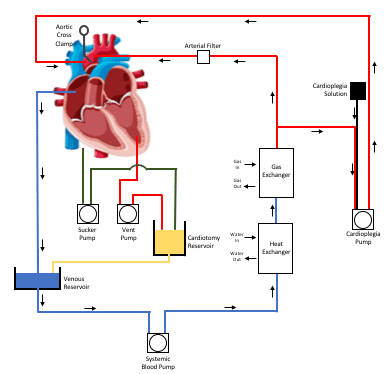
Figure 3 – Diagrammatic representation of a ‘closed’ extracorporeal circuit for cardiopulmonary bypass
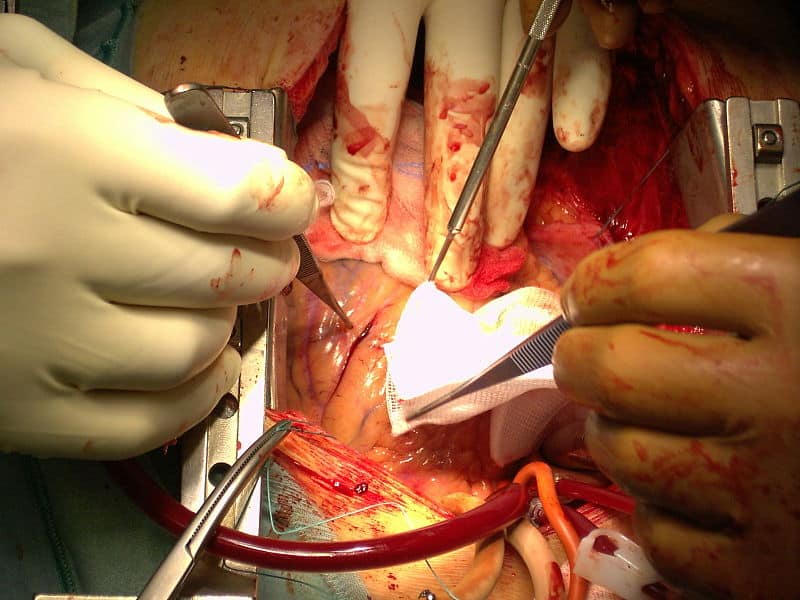
In order to maintain an effective and safe CPB circuit, good communication is essential between the surgeon, anaesthetist, and perfusionist (Fig 2). Rate of blood flow will vary depending on the stage of operation and how the patient responds to coming off bypass.
Protamine is administered at the end of the procedure to reverse the effects of heparin, but this must be done slowly to reduce cardiovascular disturbance.
Cardioplegia
Cardioplegia is the main form of myocardial protection. The cardioplegic solution used during CPB contains a high concentration of potassium chloride, which causes a reduction in resting membrane potential and excitability, resulting in cardioplegia.
It is essential that the blood flow to the myocardium is interrupted during surgery, otherwise the metabolic demand of the myocardium would far exceed the blood supply available, leading to ischaemia.
Cardioplegic solution will be topped up throughout the procedure, but is washed out at the end of the operation when the cross clamp is removed to enable recovery of myocardial electrical activity.
Complications
The potential emergency complications of CPB that can arise as a result of being on bypass are (often remembers as 2 As, 2 Is and 2 Ps):
| Scenario | Solution |
| Air lock | Replace air with fluid |
| Arterial Air embolism | Establish retrograde cerebral perfusion |
| Iatrogenic dissection | Hypothermic circulatory arrest and repair |
| IVC tear | Hypothermic circulatory arrest and repair |
| Protamine reaction | Neutralise the effect |
| Pump failure | Replace pump |
Table 1 – Potential Emergency Complications of CPB
Key Points
- Cardiopulmonary bypass takes over the function of the heart and lungs, delivering oxygen uninterrupted to the end organs during heart-lung surgery
- Whilst there are sizeable benefits of CPB, there remain systemic side-effects that occur with its use
- The flow of blood from patient to bypass machine back to patient follows a specific sequence that maximises perfusion and minimises risk