Introduction
Brain arteriovenous malformations (bAVMs) are defects in the vascular system of the brain.
The abnormal blood vessels result from feeding arteries directly connecting to a venous drainage system, in the absence of a true capillary bed.
Brain AVMs have a prevalence range of around 10-18 per 100,000, many of which remain asymptomatic and subclinical.
The origin of bAVMs remains uncertain, although they are thought to be congenital in pathophysiology, involving dysregulation of vascular endothelium growth factor.
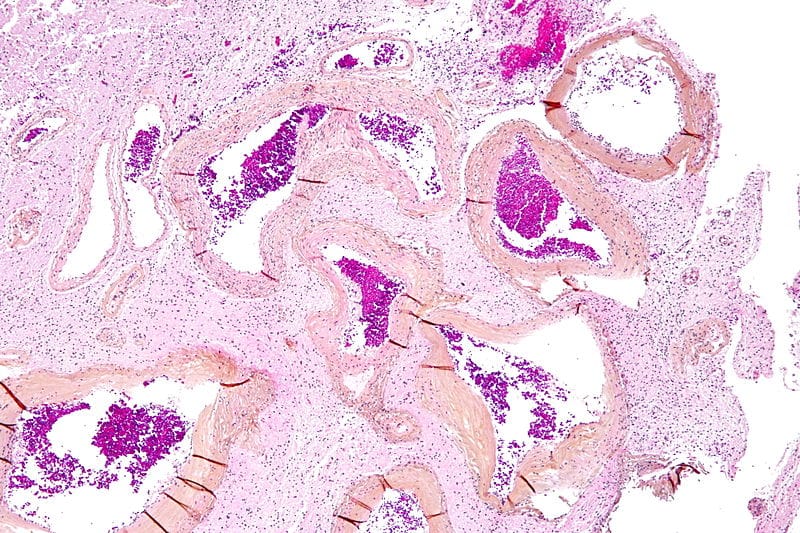
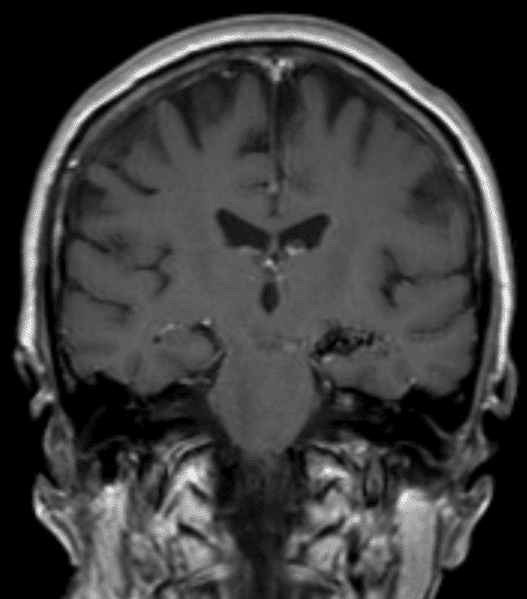
Figure 1 – Low magnification histology demonstrating an arteriovenous malformation in the brain
Classification
Brain AVMs can be classified by the Spetzler-Martin grading (SMG) system, with increasing SMG score relating to an increased morbidity and mortality of potential surgical resection.
| Size | Small (0 – 3.0cm) | 1 |
| Medium (3.1 – 6.0cm) | 2 | |
| Large (>6 cm) | 3 | |
| Location | Non-eloquent | 0 |
| Eloquent* | 1 | |
| Pattern of venous drainage | Superficial | 0 |
| Deep | 1 |
Table 1 – The Spetzler-Martin AVM Grading Scale *Eloquent locations include sensorimotor, language, or visual areas, thalamus, hypothalamus, internal capsule, brainstem, cerebellar peduncles, and deep cerebellar nuclei
A Spetzler-Ponce classification, which uses the SMG score, is used in determining management; SMG score 1-2 = Spetzler-Ponce Class A; SMG score 3 = Spetzler-Ponce Class B; SMG score 4-5 = Spetzler-Ponce Class C;
Risk Factors
No genetic, demographic, or environmental risk factors for bAVM have been established with certainty, however certain inherited disorders, such as Osler-Weber-Rendu syndrome, Sturge-Weber disease, neurofibromatosis, and von Hippel-Lindau syndrome are associated in a small minority of cases.
Clinical Features
Brain AVMs tend to be clinically asymptomatic, until the presenting event develops or being picked up incidentally on imaging*
Of those presenting symptomatically, half will present with haemorrhage. Other common presentations of brain AVMs are seizures (25%-40%), persistent headaches (20%), and focal neurology (15%).
*Brain AVMs present as an incidental finding in cerebral angiography in around 15% of patients
Investigations
Digital subtraction angiography (DSA) is the gold standard for diagnosis of bAVMs, delineating the location and number of feeding vessels and the pattern of drainage. They appear as a tightly packed mass of enlarged feeding arteries that supply a central nidus.
Both CT and MR angiography can also be used to detect bAVMs, also useful in the assessment of any potential developing complications, such as previous haemorrhage and adjacent oedema.
Once detected, transcranial Doppler imaging can be used as a reliable and non-invasive method to monitor and follow-up bAVMs.
Management
The ultimate goal of bAVM management is prevention of future haemorrhage. The Spetzler-Ponce classification of bAVM provides a guide to treatment; classically, surgery is recommended for Class A, multimodality treatment for Class B, and observation for Class C*.
Three main surgical modalities exist:
- Microsurgery has the advantage of a complete removal of an AVM in one session, eradicating the risk of recurrent haemorrhage, however is an invasive procedure
- Stereotactic radiosurgery can be effective for malformations that are smaller than round 3.5cm, but complete obliteration requires approximately 1-3 years post-treatment and cure is not always achieved
- Endovascular embolisation is used typically to facilitate subsequent surgery and is will not achieve a permanent obliteration of the AVM due to high rates of recanalisation
The most favourable operative profile is individuals <40yrs, absence of neurological deficits, superficial and small AVMs, and present in a non-eloquent area.
Prognosis
The main complication of bAVM is rupture, with rupture rates reported around 2-4% per year; of those that rupture, serious morbidity or mortality occur in over 40% of cases.
The risk of subsequent haemorrhage is also increased when the bAVM presents in acute haemorrhage, has deep venous drainage or deeply located, or is associated with an aneurysm.
Unfortunately, treatment of bAVMs remains associated with a substantial risk morbidity and mortality.
Key Points
- Brain arteriovenous malformations tend to be clinically asymptomatic, most being picked up incidentally
- Gold standard diagnosis is via digital subtraction angiography
- The main goal of bAVM treatment is prevention of haemorrhage, with management option dependent on severity and extent of disease
- Rupture is the main complication of bAVM, associated with a high morbidity and mortality