Hyperhidrosis is defined as sweating in excess of that required for regulation of body temperature.
Sweating is controlled by the autonomic nervous system. Increased sympathetic stimulation from thoracolumbar autonomic fibres stimulate the eccrine (water) sweat glands (rather than the oily apocrine glands) to increase sweat production.
Hyperhidrosis can be divided into:
- Primary – no underlying cause is present and usually localised to specific areas, such as the hands, armpits, scalp, or feet, most commonly in a symmetrical distribution
- Most cases start in the teenage years yet will improve as the patient gets older; a third of patients have a positive family history
- Secondary – associated with an underlying condition, including systemic conditions or medication, and can present with generalised sweating or focal to specific areas
Causes
Causes for secondary hyperhidrosis include:
- Pregnancy or menopause
- Anxiety
- Infections
- Including tuberculosis, HIV, or malaria
- Malignancy, especially lymphoma
- Endocrine disorders
- Including hyperthyroidism, phaeochromocytoma, or carcinoid syndrome
- Medication
- Including anticholinesterases, antidepressants, or propranolol
Clinical Features
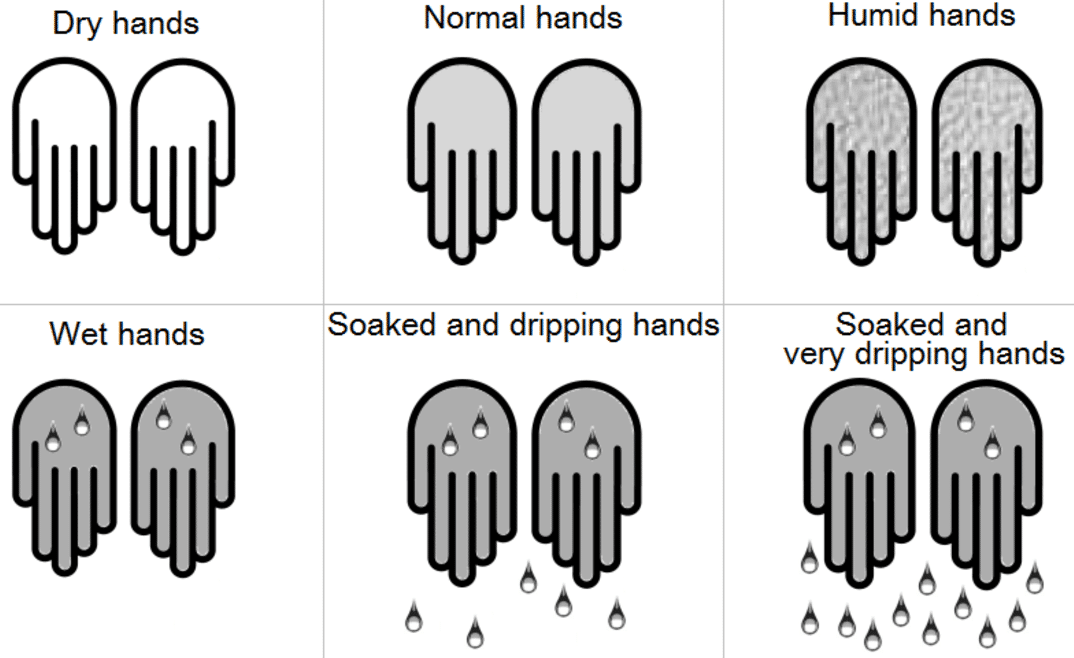
Primary hyperhidrosis will often present with focal sweating, typically bilateral and symmetrical, occurring at least once a week. It typically onsets before 25yrs of age and should be present for >6months for the diagnosis to be made.
Secondary hyperhidrosis will often be generalised sweating and in many cases predominantly at night time*. It is important to assess for features of underlying secondary causes, such as pyrexia, palpitations, or unexplained weight loss.
*Interestingly, many cases of primary hyperhidrosis will stop during sleep
Investigation
Diagnosis of primary hyperhidrosis is often made through history and examination, yet secondary causes should be excluded first
Blood tests, including FBC, CRP, U&Es, TFTs, and glucose, and a CXR are typically done as routine, however more focused specialist tests will be dependent on the patient presentation.
Management
Most patients should be given initial lifestyle advice, such as reducing stress or anxiety, avoiding spicy food, and using absorbant underlayers or armpit pads. Loose fitting clothes of natural fibre and leather shoes can also help.
Anti-perspirants from over the counter can be used initially, however use of aluminium chloride (applied at night only) can also be trialled (although this can often cause painful and erythematous skin in the areas applied)
Propantheline is the only anticholinergic agent licenced for use in hyperhidosis. Glycopyrrolate and oxybutynin (also anticholinergic agents) can reduce sweating but not readily available and are often off-license.
Surgical Intervention
For those patients with resistant symptoms significantly affecting quality of life, a few surgical interventions* are available:
-
By TeachMeSeries Ltd (2020)
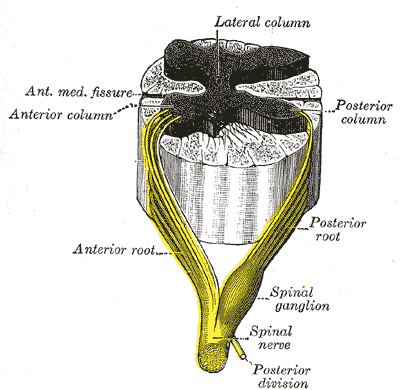
Figure 2 – Spinal ganglia are damaged specifically in an attempt to reduce the symptoms of hyperhidrosis in ETS
Iontophoresis involves use of a weak electrical current through the area through water soaked sponges
- Only a short-term solution, likely works by a combination of blocking sweat glands, disrupting nerves, and making sweat more acidic
- Botulinum toxin can be injected into the skin in very small doses to block the nerve supply to the sweat glands.
- Its effect lasts around 2-6 months and can be repeated, however only licensed for underarm but not for hands or feet as this can result in weakness.
- Endoscopic thoracic sympathectomy (ETS) involves causing damage to the thoracic sympathetic ganglion (Fig. 2) supplying the affected region (most useful for palm and face involvement)
- This is a major operation with the risk of damaging other nerves or the lung parenchyama, hence should only be done as a last resort
*Many patients who receive treatment often develop to compensatory sweating in another locations, hence is a side effect that patients must be informed of
Key Points
- Hyperhidrosis is defined as sweating in excess of that required for regulation of body temperature
- May be primary or secondary in aetiology
- Diagnosis of primary hyperhidrosis is made through history and examination, yet secondary causes should be excluded
- Most cases can be managed medically, however surgical interventions are possible for resistant cases