Introduction
Penile cancer is a rare urological cancer. Around 630 men are diagnosed each year in the UK, although higher rates are seen in Africa, South East Asia and South America. It is most commonly diagnosed in men over 60yrs.
Penile cancer has a strong association with Human Papillomavirus (HPV), specifically subtypes 16, 6, and 18, with around one third to half of all cases associated with HPV-related carcinogenesis
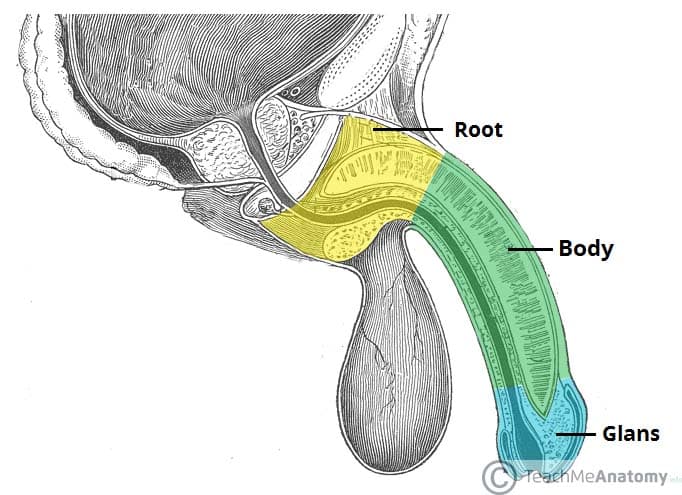
The most common penile malignancy is squamous cell carcinoma (SCC), usually arising from the epithelium of the inner prepuce or the glans, and accounts for 95% of cases (Fig. 2). Other types include basal cell carcinomas, sarcomas, melanomas, or urethral carcinoma.
Risk Factors
The most important risk factor for penile cancer is HPV infection.
Other risk factors include phimosis, smoking, lichen sclerosis, untreated HIV infection (around 8 times increased risk), or previous Psoralen-UV-A Photochemotherapy (PUVA) treatment (used for some forms of psoriasis and cancer).
Circumcision is deemed protective; indeed, penile cancer is virtually unknown in patients who have been circumcised as a child
Clinical Features
Penile cancer typically presents as a palpable or ulcerating lesion on the penis. They are most commonly located on the glans, however can be found on the foreskin, penile shaft, and scrotum. The lesions are typically painless, however the lesions may discharge or be prone to bleeding.
On examination, inguinal lymphadenopathy is present in 30-60% on cases at diagnosis, however not all demonstrate malignant infiltration (the remainder are presumed to represent an inflammatory reaction). Distant metastases are uncommon at presentation, only in 1-10% of patients.
Differential Diagnosis
There are a wide range of differentials for individuals presenting with ulcerating lesions on the penis.
Infections form the mainstay, including Herpes Simplex or Syphilis, whilst inflammatory conditions, such as psoriasis, lichen planus, or balanitis, should also be considered.
Premalignant conditions include Condyloma acuminatum (genital warts), Bowens disease, or Lichen sclerosus.
Investigations
Any patient with a suspected penile cancer should be referred to a specialist regional centre for further investigation.
The mainstay of initial investigation is via penile biopsy, allowing for the confirmation of the diagnosis.
Once confirmed, inguinal lymphadenopathy should be determined, typically using PET-CT imaging (especially in those with palpable nodes). For those with positive inguinal lymph nodes, CT imaging of the chest-abdomen-pelvis is required for complete staging.
The TNM staging system is used to classify the stage of penile cancer, as well as help establish an appropriate treatment plan.
Management
The aim of treatment is complete tumour removal and oncological control, whilst ensuring as much organ preservation as possible. Management often requires a combination of surgery, radiotherapy, and chemotherapy.
Those with superficial non-invasive disease can be treated with topical chemotherapy agents, such as imiquimod or 5-fluorouracil (5-FU), then followed up with repeat biopsy and long term surveillance is advised prior to commencing treatment.
Other treatment options include laser treatment (to ablate the tumour) or glans resurfacing (consisting of complete removal of the glandular epithelium down to the corpus spongiosum, followed by reconstruction with a split skin or buccal mucosa graft).
Surgical Management
Most cases of penile cancer will need surgical management. Traditionally a 2cm, tumour-free margin has been recommended, however a 5mm margin is considered safe.
For those with invasive disease confined to the glans, organ sparing treatment can be performed. Options include local excision, partial glansectomy (Fig 3), or total glansectomy with reconstruction (using a split skin graft). Radical circumcision may be used for purely foreskin tumours.
Treatment options for invasive penile cancer include partial amputation (removing glans penis with or without a portion of the underlying corpora) with reconstruction, or total penectomy (removal of glans penis and most or all of the underlying corporal bodies) with perineal urethrostomy. Neoadjuvant radiotherapy or chemotherapy may also be required.
Those with inguinal node involvement may require radical inguinal lymphadenectomy, neoadjuvant chemotherapy, or radiotherapy (in palliative cases).
Reconstruction Options
Once the patient is disease free for a suitable time, phallic reconstruction is possible by forearm phalloplasty.
Prognosis
Penile cancer remains a largely treatable disease, with an 85% 5-year survival rate for those diagnosed at the T1 stage, however reduced to 12% if there are distant metastases at presentation. The overall 5-year survival rate for penile cancer is around 70%.
Key Points
- Penile cancer is a rare urological cancer, and has a strong association with Human Papillomavirus
- Penile cancer typically presents as a palpable or ulcerating lesion on the penis
- Diagnosis is made through tissue biopsy and CT imaging
- Management often requires a combination of surgery, radiotherapy, and chemotherapy
- The overall 5-year survival rate for penile cancer is around 70%