Introduction
The nail is an essential component of the fingertip. It acts to protect the fingertip and provides counterforce to the pulp, allowing for fine and precise movements.
Nail bed injuries are common, involving younger patients with a 3:1 male-to-female predominance. Crush injuries from doors, machinery, and heavy equipment are the most frequent presentation.
The extent of damage is dependent upon the mechanism and force involved. Nail bed injuries may result in subungual haematoma formation, laceration or avulsion of the nail bed, underlying bony fracture, or even vascular compromise to the distal fingertip.
Pathophysiology
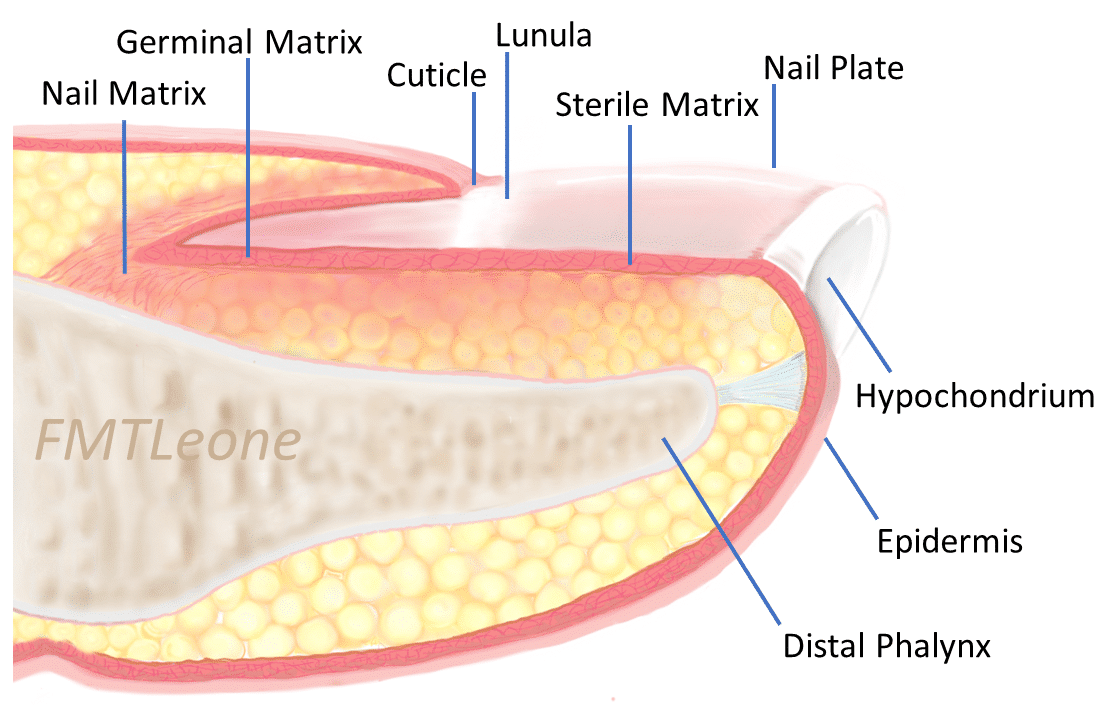
The nail bed is made up of soft tissue and is bound to the underlying periosteum of the distal phalanx.
It consists of the germinal and sterile matrix, which are responsible for nail growth. The germinal matrix lies proximal to nail plate and is responsible for approximately 90% of nail plate growth. The sterile matrix lies distal to the germinal matrix and provides the remaining 10%.
Nail bed injuries are most commonly caused by crush injuries. Crushing trauma to the nail bed can cause compression of the nail, nail bed, or bony surface. Damage to a specific region of the nail bed can give characteristic changes during regrowth to the nail for example, a scar in the germinal or sterile matrix can result in a split or absent nail.
Types
Subungual Haematoma
A subungual haematoma forms when blood collects between the nail and nail bed (Fig. 2). The colour of the haematoma can change from red/purple to brown/black giving it a bruise-like appearance.
The formation of a subungual haematoma is often related to heavy impact such as a door crush injury or a heavy weight falling on the finger.
Nail Bed Laceration
Compression of the nail bed between the distal phalanx and nail can result in a simple or complex laceration. A nail bed laceration is usually present with an intact nail and a subungual haematoma greater than 50% of the nail surface area. Sharp objects like knives can penetrate the nail if they land with sufficient force resulting in a nailbed laceration.
Nail Bed Avulsion
A nail bed avulsion is when the nail and part of the nail bed are pulled away from the rest of the finger. This is usually caused by higher energy injuries with traction and crushing forces. Avulsion injuries most commonly occur in the ring finger and are often associated with other injuries, such as distal phalanx fractures and dislocations.
Clinical Features
Patients with nail bed injuries will present with pain following an episode of trauma. There may be associated soft tissue swelling or lacerations to the surrounding skin. Depending on the severity of the injury, underlying distal phalanx fractures may also be present.
On examination, it is important to inspect the posture of the finger to rule out any additional injuries, such as tendon avulsions or fractures / dislocations. Ensure to complete a neurovascular examination; the injured nail can be examined under a digital nerve block if the patient is in severe pain.
Differential Diagnosis
The main differential diagnoses to consider include distal phalanx fracture, fingertip amputation, fingertip infection, foreign bodies, neuroma, or phalangeal dislocation.
Investigations
Most cases can be diagnosed clinically however plain film radiographs of the injured finger should be taken to rule out fractures, dislocations, and foreign bodies.
Anteroposterior, lateral, and oblique views of the injured finger are commonly used to rule out distal phalanx fractures (and Seymour growth plate fractures in children).
Management
The management of nail bed injuries will depend on the type and extent of injury sustained. Following initial assessment and irrigation, simple nail bed injuries may be managed conservatively, often with a short course of prophylactic oral antibiotics.
Most nail bed injuries will require removal of the nail plate, nail bed repair, and splinting of the eponychial fold. The nail plate is carefully separated from the underlying sterile and germinal matrix soft tissue and soaked in betadine solution.
Nail bed repairs are undertaken usually with a 6-0 absorbable suture, such as Vicryl Rapide. The removed nail plate may then be trimmed and used to splint eponychial fold to facilitate growth of the new nail plate.
Prognosis
With appropriate treatment, many injuries to the nail bed make a full recovery although it can take months for the nail to grow back normally.
Injuries that are isolated to one to two thirds of the nailbed normally fare better than those that span the entire nail bed. Avulsion injuries and injuries associated with distal phalanx fractures have a worse prognosis.
Common complications of nail bed injuries include scarring, infection, hook nail, and split nail* (caused by scarring of the matrix).
*Treatment for scar nail is to excise the scar tissue and can even replace the nail matrix with a graft; treatment for hook nail is to remove the nail and trim the matrix to the level of the bone
Key Points
- The main types of nail bed injuries include subungual haematoma, nail bed laceration, and nail bed avulsion
- Most cases can be diagnosed clinically however plain film radiographs of the injured finger should be taken to rule out fractures, dislocations, and foreign bodies
- The management of nail bed injuries will depend on the type and extent of injury sustained
- With appropriate treatment, many injuries to the nail bed make a full recovery