Introduction
Malignant lesions of the liver represent metastasis from other primary cancers in 90% of cases, with primary liver malignancies being relatively rare. Of the primary liver cancers, 90% are hepatocellular carcinoma (HCC), with intrahepatic cholangiocarcinoma making up the remainder.
Hepatocellular carcinoma is the sixth most common cancer worldwide and the second leading cause of cancer death. Incidence rates vary significantly across the globe, mainly determined by the incidence of hepatitis B virus (HBV) and hepatitis C virus (HCV) infection; in China there are over 400 cases per 100,000 people, whilst in the UK there are just around 13 cases per 100,000 people.
In the UK, the majority of cases occur in those >70 years old with around 65% of cases occurring in males; in areas of high endemic HBV or HCV infection rates, age of diagnosis is much lower.
Aetiology
HCC generally arises as a result of a chronic inflammatory process affecting the liver, with 80-90% of cases seen on a background of established liver cirrhosis.
The aetiology of the inflammation is mainly due to viral hepatitis, however other causes for HCC are chronic alcohol excess, hereditary haemochromatosis, primary biliary cirrhosis (PBC), and aflatoxin exposure (a toxic fungal metabolite)
Risk Factors
The main risk factors for developing HCC are:
- Liver cirrhosis
- Viral hepatitis infection, mainly hepatitis B virus and hepatitis C virus, alcohol excess, non-alcoholic fatty liver disease, and other rare causes including metabolic (hereditary haemochromatosis, Wilson’s disease) and autoimmune (primary biliary cirrhosis) processes
- Aflatoxin exposure
- Particularly in combination with HBV infection
- Hepatocellular adenoma*
- Smoking
- Advanced age (>70yrs)
- Positive family history
*Approximately 5% risk of malignant transformation in women with lesions >4cm and 50% in men with lesions of any size
Clinical Features
Many cases in developed countries are picked up on surveillance imaging, in those patients identified as high risk (e.g. known liver cirrhosis patient).
Less commonly, patients may present with non-specific systemic symptoms, such as fatigue or weight loss. Abdominal pain* in HCC is uncommon, especially in early stages of the disease.
On examination, classically an irregular enlarged liver is palpable, however in early HCC disease, this may not be present. Those with already established liver disease may present with features of decompensated liver disease, such as ascites, jaundice, or confusion.
*Tumour rupture is seen in a small number of patients, with either pain secondary to bleeding or, more rarely, haemodynamic compromise
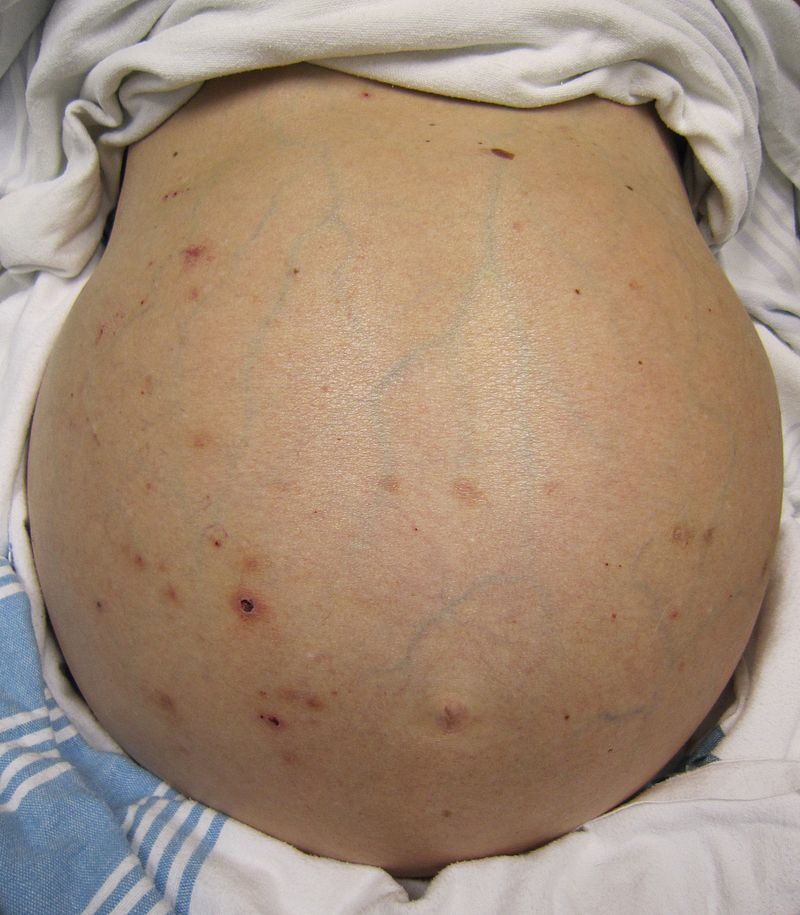
Figure 2 – Ascites, an indicator of late stage liver disease.
Investigations
Laboratory Tests
A patient with suspected HCC should have routine bloods, including full blood count, liver function tests and a clotting profile.
An alpha fetoprotein (AFP) level should be measured in all suspected cases, but is frequently not elevated in confirmed cases, and is most useful as measure of disease response or surveillance in previously diagnosed patients.
Imaging
Ultrasound scanning is the initial imaging modality of choice for screening of HCC in high-risk individuals. HCC lesions show as hypodense heterogenous lesions on ultrasound, however are often difficult to distinguish from any background cirrhosis if present.
Contrast-enhanced ultrasound (Fig. 3) has been used to investigate arterialisation of hepatic lesions in order to aid diagnosis of HCC in suspicious lesions.
MRI imaging or CT imaging (Fig. 4) are both useful to further assess lesions identified by ultrasound. These imaging modalities typically show the mass with vivid enhancement during the late arterial phase and a subsequent rapid wash out.
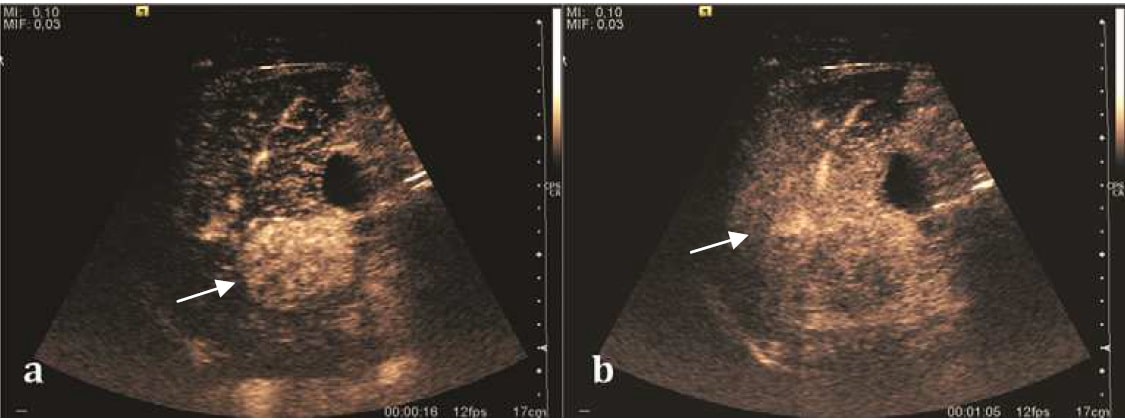
Figure 3 – A contrast-enhanced ultrasound of a hepatocellular carcinoma
In cases well characterised and with typical imaging features of HCC, diagnosis can be made radiologically. Where these requirements are not met, biopsy can be obtained for histological diagnosis, by either ultrasound-guided or CT-guided percutaneous biopsy. This should be undertaken in a centre with experience, due to the risk of tumour seeding along needle tracts (1-5%).

Figure 4 – A CT scan demonstrating a hepatocellular carcinoma
Staging
The Barcelona Clinic Liver Cancer staging system (BCLC) is the most accepted and widely used staging for HCC. It accounts for tumour stage, based on tumour size and number of tumours, as well as liver function*, physical status, and cancer related symptoms. These factors are used to define stage as 0 (very early), A (early), B (intermediate), C (advanced) and D (terminal) with further characterisation allowing definition of treatment plan and prognostication.
*The liver function is largely defined by Childs-Pugh score, which derives a score from serum bilirubin and albumin levels, INR, and the presence and degree of any ascites and hepatic encephalopathy
Management
Treatment for hepatocellular carcinoma should be decided by discussion by a multidisciplinary team, including hepatology, hepatopancreaticobiliary surgery, diagnostic and interventional radiology, and medical oncology.
Treatment options can be categorised as local or systemic and curative or palliative. Curative options include surgery, in the form of liver transplantation or liver resection, along with ablative techniques using microwave or radiofrequency ablation. Liver transplant removes the underlying aetiology for HCC in cirrhotic patients and therefore risk of recurrence is very low, whilst liver resection and ablative therapies do not address cirrhosis and recurrence is often seen in remnant parenchyma.
In those with metastatic disease, systemic therapies are indicated, namely anti-angiogenic agents such as Sorafenib and Atezolizumab. These therapies are also used in patients with diffuse intrahepatic disease not suitable for transplant, resection, ablation or embolisation.
Surgical Management
Surgical resection with lymphadenectomy is the treatment of choice in those with no or very mild liver cirrhosis, who do not meet criteria for liver transplantation. This can may be either anatomical or non-anatomical (wedge) resections, depending on tumour size and location. Approximately 15% of HCCs are considered suitable for surgical resection, mainly in those with unifocal disease.
After resection, the remnant liver must be a minimum of 20-40% of total liver volume, to mitigate the risk of post-hepatectomy liver failure. Remnant volume can be maximised by pre-operative portal vein embolisation to the portal vein supplying the side of the liver to be resected. After resection, the liver is able to regenerate to the size required.
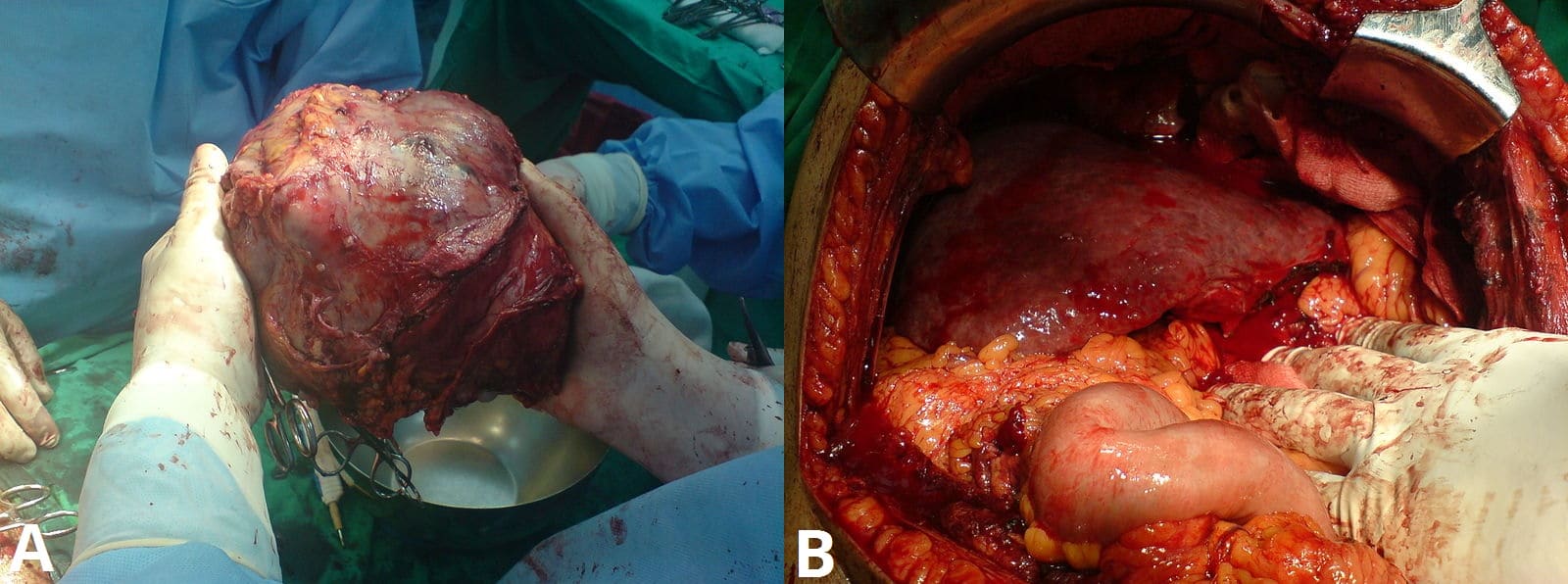
Figure 5 – Left lobe liver tumour in a 50yr old male (A) removal of the tumour (B)the liver after resection
Liver transplantation is used only in cases which meet the Milan criteria:
- One lesion < 5cm or up to three lesions all <3cm
- There is no vascular infiltration
- There are no extra-hepatic manifestations
Using these criteria, liver transplantation gives a 60-75% 5 year survival. Liver transplant carries a significant post-operative mortality of approximately 10%, and will also require lifelong immunosuppression. Most patients will also have significant time on the transplant waiting list due to shortages of donor organs, therefore may need interim treatments to prevent progression, such as resection, ablation, or chemoembolisation.
Non-Surgical Management
Ablation
Ablation may be carried out percutaneously under image guidance, or at surgery, normally when other lesions are being resected, as part of a hybrid procedure. Ablation is suitable for tumours up to 3cm in size with no more than 3 tumours, with no or mild cirrhosis, and the tumours must be visible on ultrasound or CT to allow probe placement.
Ablation is best used for deep-sited small tumours, which would require major hepatectomy for resection and for patients not considered fit for surgery. Ablation is most commonly carried out by radiofrequency (RFA) or microwave (MWA); cryoablation and injection of alcohol has been performed but are less effective.
There are no sizeable differences in outcomes between resection and ablation for early HCC. Ablation may therefore be used as a primary curative treatment, as well as a neoadjuvant treatment for those awaiting liver transplant.
Transarterial Chemoembolisation
HCCs receive almost all blood supply from the hepatic arterial system (as opposed to portal venous like normal hepatic parenchyma). Transarterial Chemoembolisation (TACE) exploits this by selective embolisation of arteries feeding tumours, leading to tumour ischaemia and necrosis.
Embolisation is achieved by injection of chemotherapy along with an embolising agent under radiological guidance into superselected arteries supplying tumours. TACE is reserved for patients with BCLC stage B, with well defined tumour nodules not suitable for resection or transplant. Whilst it is not curative, TACE has been shown to improve survival and is associated with low morbidity.
Prognosis
The prognosis of hepatocellular carcinoma depends on the extend of the underlying cirrhosis, as this plays a large role in determining how aggressively the cancer can be treated, as well as the patient’s liver disease burden.
The expected 5 year survival for each treatment pathway, assuming no or mild cirrhosis, are:
- Liver transplantation 60-75%
- Liver Resection 45-70%
- Ablation 68% (in tumours <2cm)
- TACE 26%
Secondary Liver Metastases
Approximately half of metastasis to the liver arise from colorectal primary tumours, due to spread via the portal circulation. However, any solid organ tumour can metastasise to the liver with pancreas, breast and lung being the next most common.
These are typically picked up on staging imaging following the initial diagnosis. However, patients can present with jaundice or right upper quadrant pain.
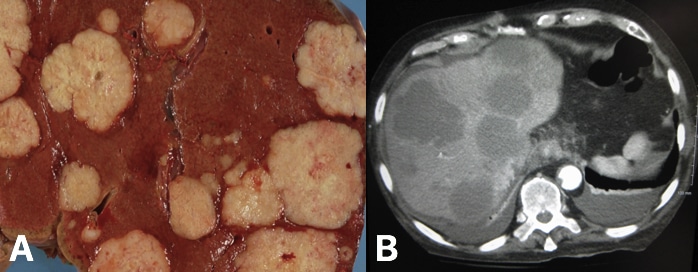
Figure 6 – Metastatic liver (A) metastatic liver deposits from a colon primary, seen on post-mortem (B) CT scan showing metastatic liver deposits
Historically, patients with liver metastases from any primary were considered incurable and palliation was the mainstay of treatment. However, now colorectal metastasis (as well as metastases from melanoma, neuroendocrine tumours (NETs), testicular cancer, or ovarian cancer) may be considered for surgical therapy to improve survival.
Treatment options for liver metastases are broadly similar to those for primary liver tumours, with surgical resection, ablation, and TACE all being possible. In a small number of selected cases, mainly NETs, liver transplantation may be considered.
Resection with curative intent is considered whereby a large enough functional liver remnant can be maintained whilst achieving oncological clearance of disease.
Key Points
- Hepatocellular carcinoma (HCC) is most commonly associated with cirrhosis secondary to hepatitis virus infection or excessive alcohol intake
- AFP levels are most useful for monitoring of response to treatment and recurrence
- Management and prognosis can be determined by the Barcelona Clinic Liver Cancer staging system
- Both surgical and non-surgical options may be curative and include liver resection or transplantation and ablation
- The most common cancers that metastasise to the liver are those from bowel, pancreas, breast, and lung