Introduction
Intracranial infections are infections of the central nervous system (CNS) that can be caused by bacteria, viruses, or fungi. They form an important differential diagnosis in those presenting with rapidly progressive neurological illness or systemic manifestation of sepsis with an unclear source.
A delay in recognising CNS infections in the emergency setting can result in severe morbidity and death. The main types of intracranial infections include meningitis, extradural abscess, subdural empyema, and cerebral infections (cerebral abscess, encephalitis, or ventriculitis); surgical intervention can be required in extradural abscess, subdural empyema, and cerebral abscess.
The main routes of spread for pathogen to cause these infections are (1) haematogenous spread via the choroid plexus, (2) direct extension from adjacent tissues, and (3) inoculation from interventional procedures or surgery. Within the cerebral vasculature, infiltration of peripheral immune cells is restricted by the blood-brain barrier (BBB), therefore once pathogens have entered the CNS, they can rapidly progress and spread.
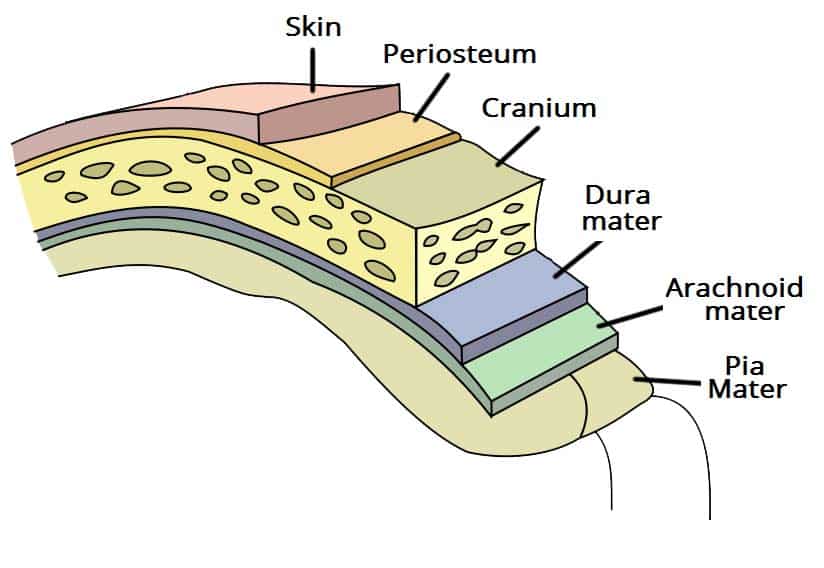
Extradural Abscess
An extradural abscess typically develops following neurotrauma, surgery (such as following a craniotomy), or direct spread from sinusitis or mastoiditis. The condition often presents with localised pain over the affected region and can present concurrently with osteomyelitis of the cranial vault. The most common causative organisms are Streptococci and S. aureus.
Subdural Empyema
A subdural empyema typically develops as direct spread from sinusitis (particularly frontal sinusitis) or from chronic otitis media, extending to the subdural space via the emissary veins or as a result of retrograde thrombophlebitis.
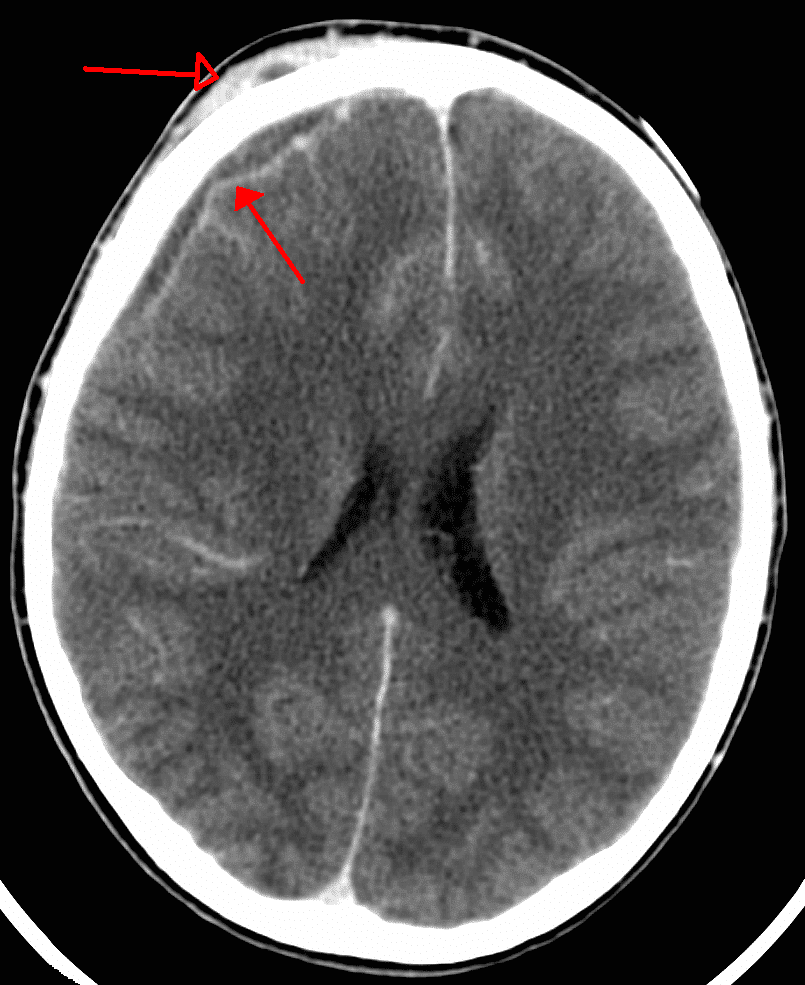
Figure 2 – CT scan showing a subdural empyema (filled arrow), with a concurrent extracranial skin abscess
Cerebral Abscesses
A cerebral abscess can occur due to direct spread from sinusitis, haematogenous spread from a septic focus*, or following a penetrating wound to the head or following neurosurgical procedures.
The most common causative pathogens are S. pneumoniae and S. aureus. On cross-sectional imaging, cerebral abscesses will present as discrete lesions with an enhancing rim (Fig. 3).
*Conditions that can cause septic emboli resulting in cerebral abscess include infective endocarditis or patients who are intravenous drug users
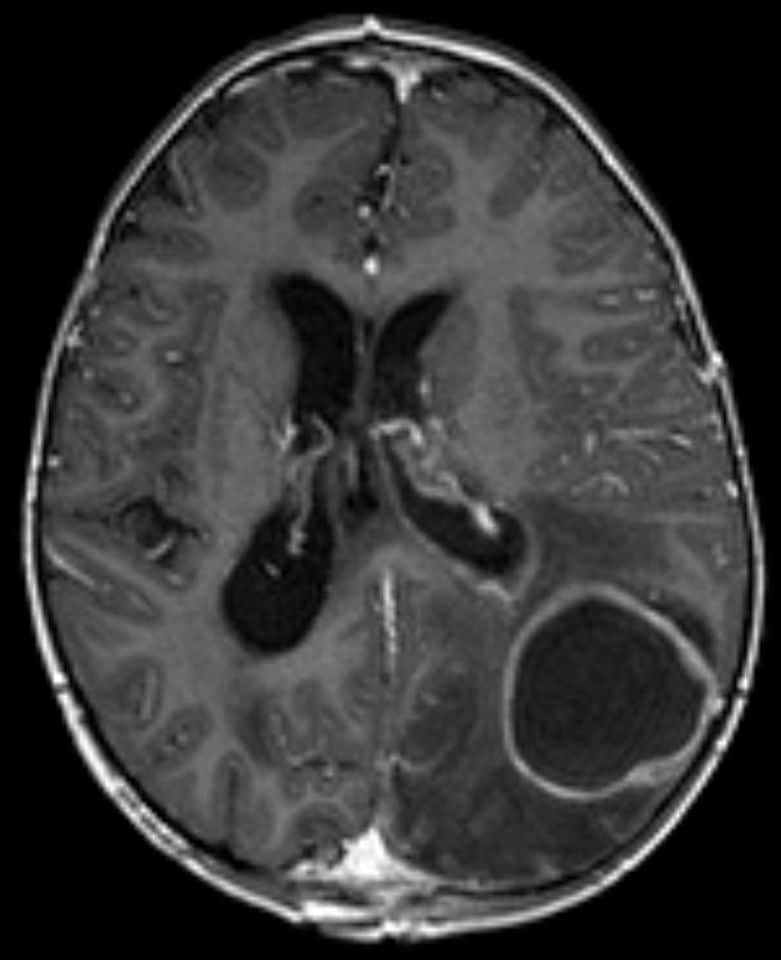
Figure 3 – MRI imaging (in T1 weighting) demonstrating a cerebral abscess
Ventriculitis
Ventriculitis is characterised by inflammation of the ependymal cells which lines the cerebral ventricles. It often develops secondary to pre-existing infections (e.g. meningitis), however may develop from those with external ventricular drains (EVD) in-situ or following intracranial surgery.
Clinical Features
The clinical features of CNS infections vary with each underlying pathology, however in general they will present with new-onset confusion or reduced level of consciousness, headache, or clinical features of sepsis.
Intracranial abscesses can result in features of mass effect, including raised intra-cranial pressure, or seizure activity. On examination, patients will often have reduced or fluctuating consciousness, persistent pyrexia, or focal neurological deficits.
Risk Factors
The main risk factors for CNS infections include extremes of age, recent neurosurgical procedure, intravenous drug use, the presence of any long-term intracranial devices, or immunosuppresion.
Investigations
All patients with a suspected intracranial infection should have routine bloods, including FBC, U&Es, CRP, and a clotting screen, and blood cultures (especially if clinical features of sepsis present). In cases where a patient has indwelling intracranial catheters, such as a ventriculoperitoneal (VP) shunt, CSF samples can be obtained through a shunt tap procedure and should be sent for MCS.
The vast majority of intracranial abscesses can be diagnosed initially on CT imaging. A CT head with intravenous contrast will allow for characterisation of the majority of infections, however in certain cases an MRI head with gadolinium contrast (Fig. 3) may be required for better assessment and to guide treatment.
Management
Patients with intracranial infections are often very unwell, therefore ensure appropriate fluid resuscitation is provided promptly and involvement of intensive care teams early on.
Patients should be started on intravenous antibiotics, initially empirically based on local guidelines, and early involvement of microbiology is essential. Due to the blood-brain barrier, not all anti-microbial agents have good CNS penetration* and often high-dose long-term antibiotic regimes are required. Any suspected viral or fungal involvement will require appropriate antiviral or antifungal therapy respectively
Further medical adjuncts to surgical treatment include hyperosmolar agents (such as mannitol or hypertonic saline), if the patient presents with features of raised intracranial pressure, and anti-epileptic medications, if seizures are a feature of the patient’s presentation.
*For ventriculitis, an external ventricular drain is present, this can be used to administer intrathecal antimicrobials directly into the ventricular space for more localised therapy
Meningitis and Encephalitis
Meningitis and encephalitis are primarily treated medically with antibiotics. However, sometimes surgical intervention is required. For example, when the aetiology of encephalitis is unclear, brain biopsy can be performed for diagnostic purposes. Meningitis can result in hydrocephalus and raised intracranial pressure, in which case insertion of an external ventricular drain can be used to manage the patient.
Surgical Management
Definitive management of intracranial abscesses will typically require surgical intervention.
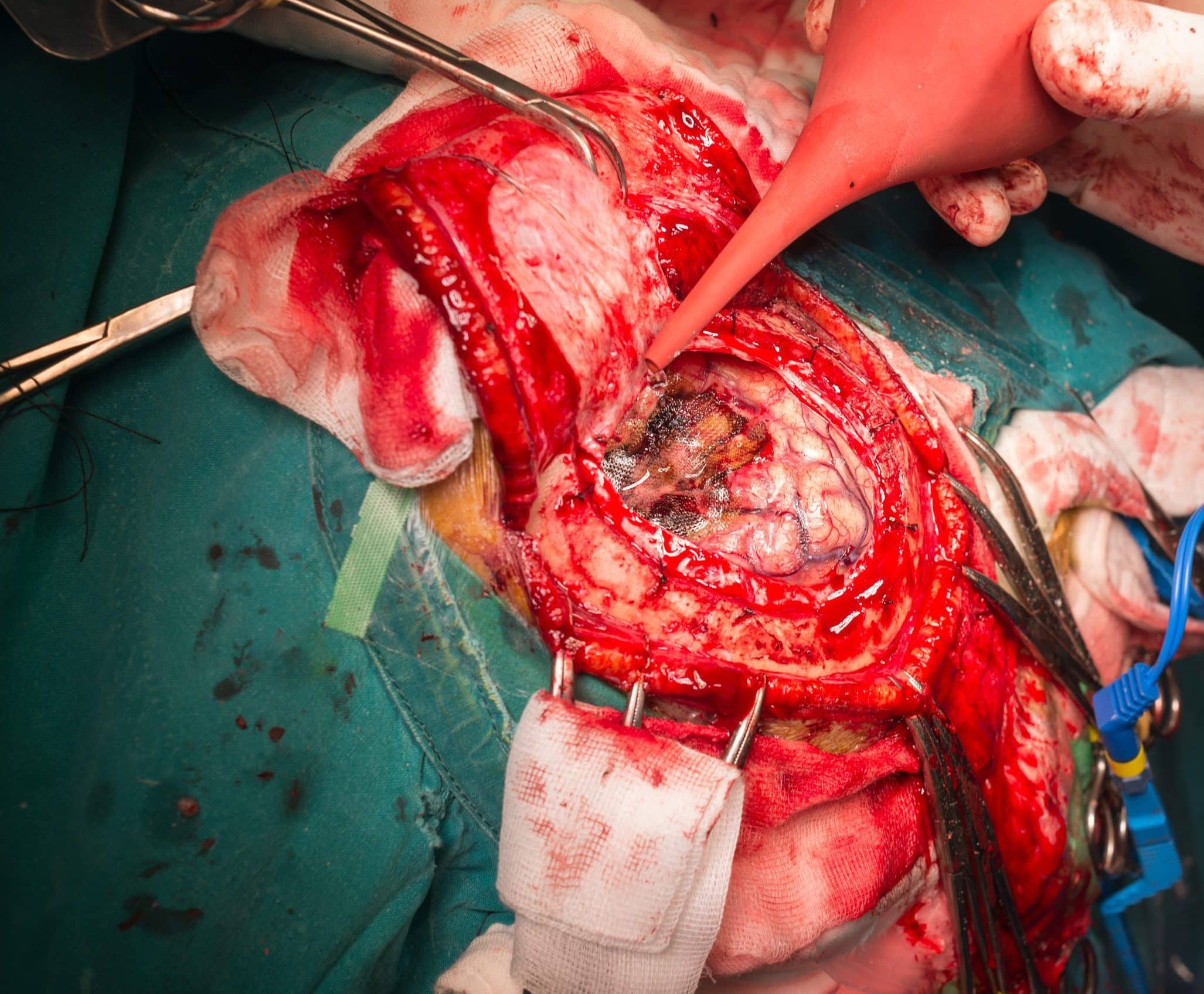
Cerebral abscesses can be drained either via a burr hole, to insert a needle into the abscess cavity to aspirate its contents (simple needle aspiration), or with a craniotomy (Fig. 4), to access and remove the abscess cavity entirely. Choosing one option over the other is based on the abscess location, patient factors, and surgical access; in all approaches, any pus obtained should be sent for culture and sensitivities to guide targeted antimicrobial therapy.
Epidural abscesses and subdural empyema may require surgical intervention, and will usually need a craniotomy to allow for thorough washout of the infected space. When caused by sinusitis or otitis media, a joint operation involving ENT surgeons may be required to control the original source of infection and reduce the risk of recurrence.
Key Points
- The main types of intracranial infections requiring surgical intervention are extradural abscess, subdural empyema, and cerebral abscess
- Patients can present with headache, pyrexia, reduction in consciousness or acute-onset confusion, or features of sepsis
- Mainstay for initial diagnosis is with a CT head scan
- Patients will require long-term high-dose antimicrobial therapy and may require surgical intervention, either via a Burr hole of craniotomy