This article is for educational purposes only. It should not be used as a template for consenting patients. The person obtaining consent should have clear knowledge of the procedure and the potential risks and complications. Always refer to your local or national guidelines, and the applicable and appropriate law in your jurisdiction governing patient consent.
Overview of Procedure
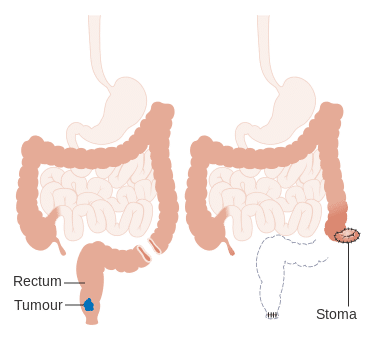
Abdominoperineal Resections (APRs) are typically performed for very low rectal cancers (or for anal cancers refractory to chemoradiotherapy) or for severe perianal Crohn’s disease
APRs have two separate stages to the procedure, with an abdominal approach (either open or laparoscopic) for the rectal dissection and end colostomy formation, and an perineal approach for the excision of the anus and completion of the rectal dissection. The entire specimen, formed of perineal skin, anal sphincters, rectum, and sigmoid colon, can then be extracted.
Complications
Intra-Operative
| Complication | Description of Complication | Potential Ways to Reduce Risk |
| Bleeding | Ensure meticulous haemostasis during the procedure; careful dissection at the splenic flexure off the spleen | |
| Damage to local structures | Structures at risk include small bowel, kidney + bladder + ureter, and ovaries + fallopian tubes + uterus | |
| Resection of other structures | Local invasion of organs may require further visceral resection, including uterus and bladder | |
| Anaesthetic risks | Includes damage to the teeth, throat and larynx, reaction to medications, nausea and vomiting, cardiovascular and respiratory complications | Forms part of anaesthetic pre-assessment |
Early
| Complication | Description of Complication | Potential Ways to Reduce Risk |
| Pain | Optimal post-operative analgesia, including epidurals or rectus sheath catheters | |
| Infection | Includes both wound infections and intra-abdominal collections, as well as respiratory or urinary tract infections post-operatively | Intravenous antibiotics at induction, minimisation of faecal contamination during procedure, wound irrigation at closure |
| Ileus | Minimise contamination and bowel handling, correct any electrolyte abnormalities post-operatively | |
| Scarring | Use of laparoscopic surgery if possible to result in a smaller abdominal scar | |
| Re-Operation | Any complication may result in the return to theatre in the immediate post-operative period | |
| DVT or PE, Myocardial Infarction, Stroke, or Mortality | As with any major surgery, whilst these events are uncommon, important to be aware of | Adequate pre-optimisation and anaesthetic assessment, peri-operative prophylactic LMWH, high-dependency level care post-operatively |
Late
| Complication | Description of complication | Potential ways to reduce risk |
| Adhesions | Attempt laparoscopic approach if possible, avoid excess tissue disruption | |
| Stoma complications | Includes stoma retraction, stenosis, or prolapse | |
| Incisional hernia, perineal hernia, or parastomal hernia | Ensure fascia is closed tightly, using a small bites techniquePlacement of perineal mesh to prevent perineal hernia | |
| Sexual dysfunction | Damage to pelvic nerves supplying the reproductive organs can be damaged during the rectal dissection, leading to sexual dysfunction |