Introduction
A haemothorax is blood entering the pleural cavity, most commonly occurring following chest trauma (Fig. 1). A haemopneumothorax is both blood and air within the pleural cavity, also typically occurring following trauma
Whilst evident in most cases, the composition of pleural fluid haematocrit must be >50% of the blood haematocrit to be formally diagnosed a haemothorax.
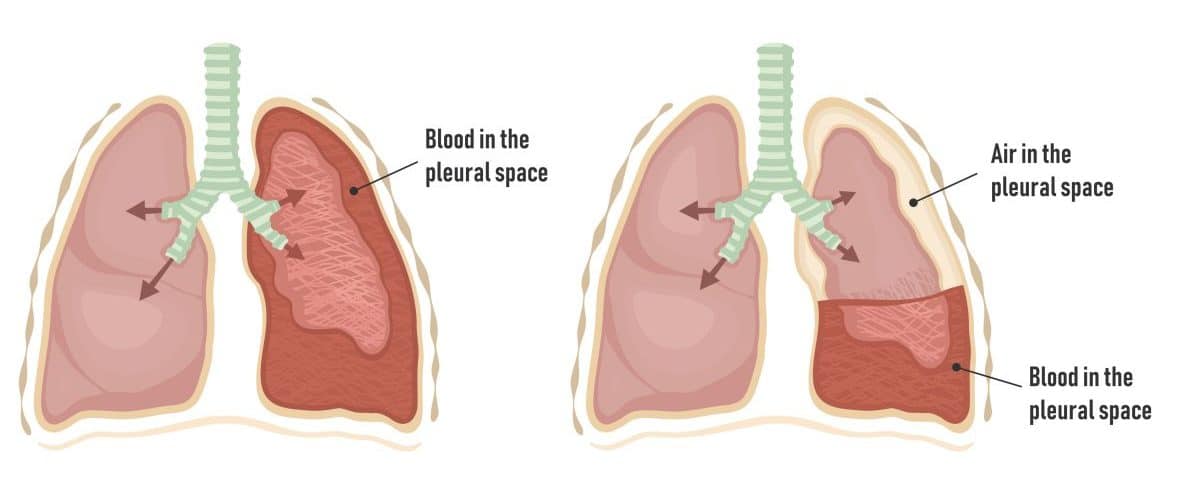
Figure 1 – A schematic showing a haemothorax and a haemopneumothorax
Aetiology
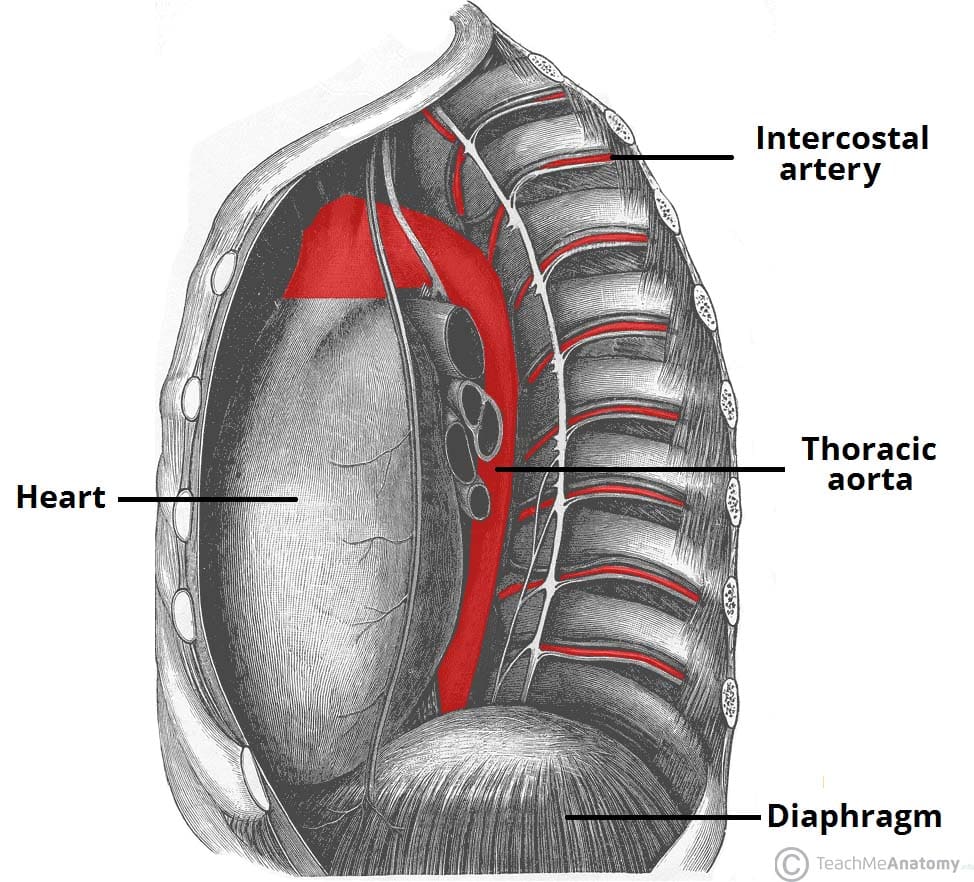
The most common cause of haemothoraces is following trauma, typically from rib fractures that damage the intercostal vessels, bleeding directly into the pleural cavity.
Less common causes include iatrogenic (e,.g. post-lung biopsies), malignancy (e.g. pleural metastasis), or disorders of blood vessels (e.g. Rendu-Osler-Weber Syndrome) or clotting (e.g. Haemophilia A).
Clinical Features
Patients will commonly present following trauma with chest pain and worsening dyspnoea. In large cases, patients can be hypoxic and hypotensive.
On examination, there will be a dullness to percussion on the affected side and reduced breath sounds on auscultation. In severe cases, there is reduced chest expansion on the affected side and potential tracheal deviation to the contralateral side.
Blunt injury may also cause bruising to the chest wall and crepitus (surgical emphysema). A flail segment may be evident in those who have sustained sizeable trauma.

Figure 3 – A large right sided haemothorax as seen on plain film chest radiograph
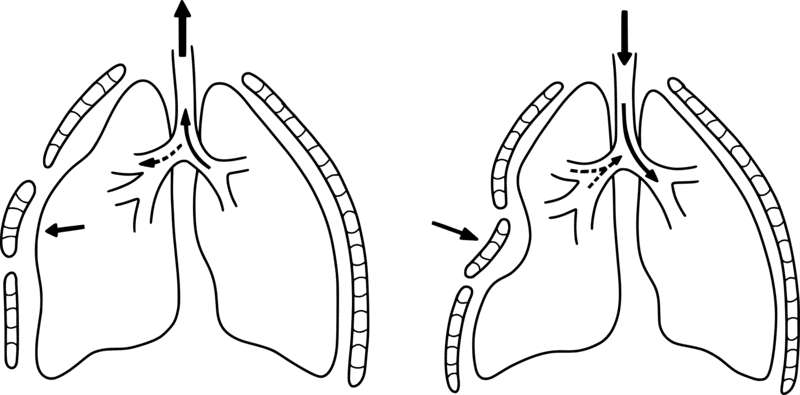
Flail Segment
Patients with multiple rib fractures can develop a flail segment if there are three or more contiguous ribs fractured in two or more places. It is often a marker of significant traumatic injury.
In a non-ventilated patient this will result in a paradoxical movement of the flail segment, whereby during expiration the segment protrudes and during inspiration the segment retracts (Fig. 4).
Investigations
Patients with suspected haemothorax should be approached in an A to E manner, following ATLS guidelines, with concurrent investigations and interventions as required. Routine bloods, including FBC, U&Es, and clotting, should be performed.
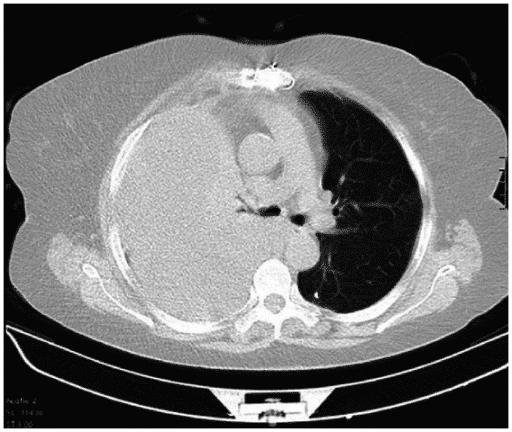
Suspected cases should have an erect plain film chest radiograph (Fig. 3) performed, in both AP and lateral views. This will show blunting of the costophrenic angle, and larger haemothorax will demonstrate a meniscus level +/- a contralateral mediastinal shift
As most cases are traumatic in nature, often patients will undergo CT imaging (Fig. 5) for the diagnosis to be confirmed, which will better characterise the size of the haemothorax and will importantly assess for other concurrent injuries
Management
Management will depend on the underlying cause, the size of haemothorax, and degree of haemodynamic stability. Ensure patients are provided with sufficient analgesia and, for trauma cases, tranexamic acid has been given (if not contra-indicated)
The majority of haemothorax require the insertion of a surgical chest drain, to evacuate the blood from the pleural cavity (Fig. 6). Large bore (28-40Fr) tubes are recommended to reduce the risk of blood clotting in the tube* and the volume from the chest drain must be carefully recorded.
Those patients with small haemothorax who are clinically stable can be admitted for observation and repeat CXR performed after 24hrs for further assessment
*If blood clotting does occur in the tube, intrapleural fibrinolytic therapy (e.g. Streptokinase or tissue plasminogen activator) may be trialled to help breakdown any clots present

Figure 6 – Plain film chest radiograph showing chest drain insertion in a patient with multiple left rib fractures and left side large haemothorax
Surgical Management
For patients with large volume blood loss (approx. >1500ml) or continuing moderate volume blood loss (approx. >200ml per hour), surgical exploration should be considered, in attempt to identify and stop the bleeding vessel. The most common procedure for this is a VATS (video-assisted thoracoscopic surgery, Fig. 7), or less commonly may warrant a thoracotomy.
Timing of VATS is crucial when evacuating a haemothorax, ideally being performed within 48-72 hours, to enable successful evaluation and early re-expansion of the lung.
If there are concurrent rib fractures, particularly with flail segments, surgical plating of the rib fractures should be considered at specialist centres to reduce pain and improve ventilation.
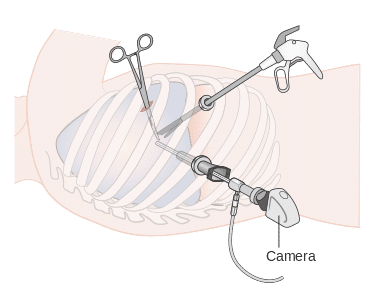
Figure 7 – Schematic demonstrating equipment for a VATS procedure
Key Points
- A haemothorax is blood entering the pleural cavity, most commonly occurring following chest trauma
- Diagnosis is made via plain film chest radiograph and typically warrants chest drain insertion
- For patients with large volume blood loss (approx. >1500ml) or continuing moderate volume blood loss (approx. >200ml per hour), surgical exploration should be considered