Acute spinal cord compression (ASCC) is a surgical emergency requiring immediate neurosurgical treatment. Prognosis of the condition can vary and is most dependent on the time between diagnosis and treatment.
In this article, we shall look at the risk factors, clinical features and management of acute spinal cord compression.
Aetiology
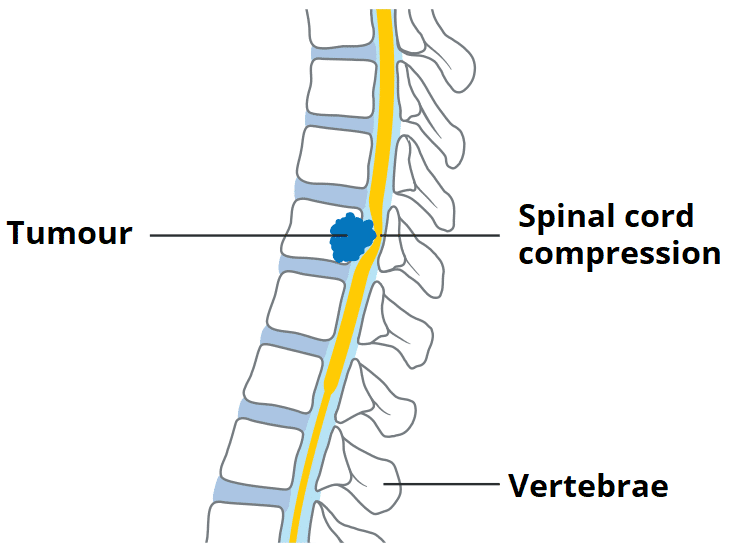
Acute spinal cord compression is caused by any pathology that leads to compression of the spinal cord. Metastatic spinal cord compression (MSCC) is the most common aetiology, however there are a wide range of causes:
- Neoplastic:
- Most commonly metastatic (MSCC) from the primary malignancies of thyroid, lung, breast, renal, and prostate; primary bone tumours, as well as haematological malignancies (e.g. myeloma) can also cause ASCC
- Traumatic:
- Typically via vertebral fracture or facet joint dislocation (although complete severance of the cord is possible)
- Infective:
- Infections resulting in abscess formation can cause compression on the spinal cord; chronic infections are typically seen with tuberculosis and fungal infections
- Disc prolapses:
- This is a rare cause of spinal cord compression, as lumbar disc herniation typically causes compression of the cauda equina inferior to the spinal cord
Any pathology that can predispose to a narrowed cord canal also lead to a greater risk of developing acute spinal cord compression. These include inflammatory conditions (such as rheumatoid arthritis or ankylosing spondylitis) or degenerative conditions (such as ligamentum flavum hypertrophy or osteophyte formation), contributing to a spinal stenosis.
Clinical Features
The history and examination are vital in differentiating acute spinal cord compression from simple disc herniation.
Sensation and proprioception will often be impaired at dermatomal levels below the cord compression. Pain can also be reported, often aggravated through straining, such as coughing or sneezing. There will be bi- or unilateral weakness in most cases (around two thirds of MSCC patients are non-ambulatory at diagnosis).
There will be upper motor neurone signs present (as opposed to the lower signs seen in peripheral nerve compression or cauda equina sydrome), including hypertonia, hyperreflexia*, Babinski’s sign, and clonus (present below the level of the lesion).
*Reflexes tend to be absent at the level of the lesion, as the lower motor neurone within the ventral horn is compressed, so producing a lower motor neurone deficit
Any autonomic involvement is a late stage and therefore carries a worse prognosis. Clinical features include bowel incontinence or constipation or urinary retention*. Additionally, there may also be evidence of the underlying cause, e.g. malignant features such as weight loss and tiredness.
*Flaccidity, although a lower motor neurone sign, is often the initial manifestation of ASCC. Over time, cord injuries at T12 or above tend to cause bladder spasticity and, below this spinal level, cause flaccidity
Differential Diagnosis
Lumbago causes pain solely around the lower lumbar area with no radiation. Sciatica will present with lower back pain spreading to the buttocks or lower limbs, depending on the dermatome affected. These both are often caused by a disc herniation pressing on the exiting nerve, producing lower motor neurone signs
Cauda equina syndrome is typically caused by a lumbar disc herniation, compressing the cauda equina. They also present with lower motor neurone signs and bladder/bowel disturbances.
Investigations
The gold standard investigation for a suspected ASCC is an MRI of the whole spine (Fig. 2). NICE guidelines recommend the imaging should be carried out within a week if spinal metastases are suggested and within a day if the cord is believed to be compressed.
Routine blood tests will be helpful, especially if the underlying cause is not apparent. Given the high chance of surgical intervention if ASCC is present, a Group & Save and clotting screen should also be taken.
Management
Especially in cases of malignancy, high dose corticosteroids can be given in an attempt to improve the patient’s functional prognosis, alongside a PPI for gastric protection.
Following imaging, an immediate referral to neurosurgery and an oncological opinion will need to be sought as required. If the patient is fit enough, surgery is the definitive treatment option for MSCC via decompression; in cases of malignancy, depending on the sensitivity of the tumour, radiotherapy and chemotherapy may also be started concurrently.
Prognosis
The prognosis of MSCC depends on the extent that the disease has progressed before decompression, as well as the underlying cause. One of the best indicators of prognosis is mobility state at the time of treatment; 90% of ambulatory patients will remain mobile, whereas only a third of non-ambulatory patients at presentation will regain an ability to walk.
Due to the nature of metastatic disease, it is likely that a patient will be in an advanced phase of cancer, if this is the underlying cause. Therefore, the survival rates for MSCC patients tend to be only approximately 6 months after the onset.
Key Points
- Acute spine cord compression is caused by any pathology that leads to compression of the spinal cord
- Clinical history and examination are important in differentiating between ASCC from a simple disc herniation
- Gold standard diagnosis is whole spine MRI
- Start high-dose steroids and seek urgent neurosurgical opinion in all suspected cases