Introduction
Thyroid lumps are a common presentation, seen in up to 5% of the population, however only a small proportion of them are cancerous.
There are different types of cancer that can affect the thyroid gland, all of which can present with different features. The main types of thyroid cancer are papillary, follicular, medullary, anaplastic, and lymphoma.

Figure 1 – Anterior view of the neck, showing the anatomical position of the thyroid gland
Thyroid Cancer Subtypes
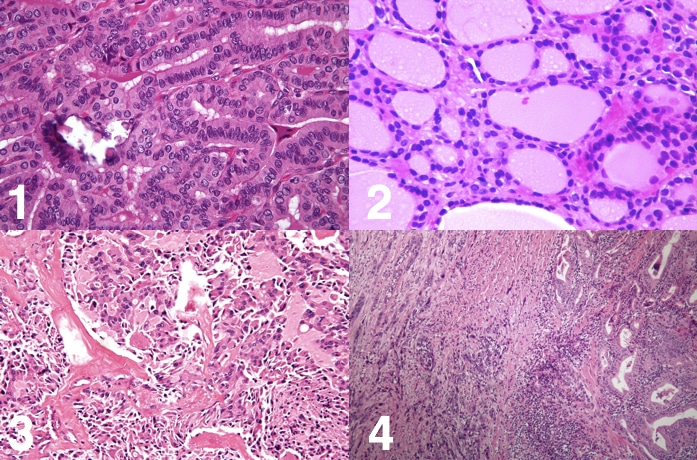
Papillary Carcinoma
This is the commonest type of thyroid cancer (75%), most commonly seen between 40-50 years and in women.
There can be multiple lesions within the gland and they are rarely encapsulated. Histologically, cells are a mixture of papillary and colloid-filled follicles, with papillary projections and pale empty nuclei. They commonly spread via the lymphatics.
Follicular Carcinoma
Usually seen at 40-60 years and in women, the second most common thyroid malignancy (15%).
They present as focal encapsulated lesions (multifocal disease is rare), with microscopic capsular invasion*. Where metastasis occurs, it is usually via haematogenous spread to bones and lungs.
*Hurthle cell tumours are a variant of follicular neoplasms in which oxyphil cells predominate
Medullary Carcinoma
These make up around 3% of thyroid cancers and arise in the parafollicular cells (C-cells, derived from the neural crest cells). Consequently, they produce raised calcitonin levels and are associated (20% of cases) with MEN 2 syndrome (both 2a and 2b).
Medullary carcinoma can spread by both lymphatic and medullary routes; unfortunately nodal disease is associated with a very poor prognosis.
Anaplastic Thyroid Cancer
These rare tumours, accounting for 5% of thyroid cancers, usually present in older patients (mean age of diagnosis 65yrs old) and are more common in women. Approximately 20% of patients with anaplastic cancer have a history of differentiated thyroid cancer.
They tend to be very aggressive, grow rapidly with early local invasion and regional or distant spread is apparent by the time of presentation in 90% of cases. Prognosis is poor and treatment is often supportive.
Lymphoma
Thyroid lymphomas are very rare, making up only 1-2% of all thyroid cancers. They usually present in people >60yrs old. Patients with Hashimoto’s disease are at higher risk of developing thyroid lymphomas.
They may grow quite rapidly, with marked compressive symptoms and B-Cell symptoms.
Risk Factors
- Female gender
- Family history – 10x increased risk for those with a first-degree relative with thyroid cancer
- Includes relevant cancer syndromes, e.g. medullary subtype associated with Multiple Endocrine Neoplasia (MEN) Syndrome type IIa and IIb
- Radiation exposure in childhood
- Full body radiotherapy for bone marrow transplant
- Hashimoto’s disease
- Predisposes to lymphoma subtype
Clinical Features
Thyroid cancers may present as a palpable lump, multiple lumps, or be found incidentally on imaging of the neck.
The red flag clinical signs to be aware of with any neck lump that may suggest a malignancy are:
- Rapid growth or pain
- Pressure symptoms, such as dysphagia
- Cough, hoarse voice, or stridor
- Multiple enlarged cervical lymph nodes
- Tethering of the lump to surrounding structures
Differential Diagnosis
It is important to remember that most lumps or swellings of the thyroid are not malignant, however some of them may still require surgical intervention for diagnosis or management.
- Benign thyroid adenoma or thyroid cyst
- Toxic multi-nodular goitre
- Toxic refers to excessive productive of thyroid hormone which results in the clinical features of hyperthyroidism
- Non-toxic multi-nodular goitre
- Thyroglossal duct cyst* (not in the thyroid itself)
- Will move superiorly as the patient sticks out their tongue
*Thyroglossal cysts, prior to any suggested removal, should be fully investigated with ultrasound thyroid as the as the cyst may be the only functioning thyroid tissue that the patient has therefore should not be removed.
Investigations
Most patients with a neck lumps should have initial Thyroid Function Tests* (TFTs) performed. Any evidence of a toxic nodule (low TSH or raised T3 or T4, or radio-nucleotide imaging showing a “hot” nodule) has a lower likelihood of malignancy.
*Serum calcitonin may be useful for the diagnosis and monitoring of treatment response in medullary carcinoma.
Most cases of suspected thyroid malignancy require ultrasound thyroid scan (Fig. 4), used to assess the nodule and look for cervical lymphadenopathy. Suspicious features on ultrasound include:
- Microcalcifications
- Hypoechongenicity
- Irregular margin
- Increased vascularity
|
Classification |
Interpretation |
|
U1 |
Normal (no nodules) |
|
U2 |
Benign nodules |
|
U3 |
Indeterminate |
|
U4 |
Suspicious features of malignancy |
|
U5 |
Definite malignancy |
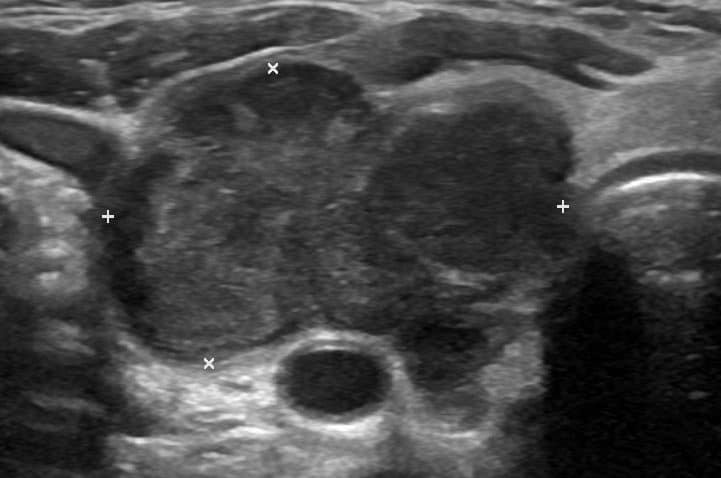
Figure 4 – Ultrasound scan showing an Anaplastic Thyroid Malignancy
Fine Needle Aspiration Cytology (FNAC) involves passing a needle into the thyroid nodule and aspirating cells out of it. These cells will be reviewed and the relevant score allocated (Thy1-Thy5); the TNM staging system is used for thyroid cancers once diagnosis is confirmed:
- Thy1 is inconclusive and requires a further sample
- Thy2 is benign lesion (may need a repeat sample if suspicious features of ultrasound)
- Thy3 is an indeterminate lesion (possible malignancy), either atypia or a follicular neoplasm, requires diagnostic hemithyroidectomy for histology to determine
- Thy4 is suspicious of malignancy and requires diagnostic hemithyroidectomy
- Thy5 is malignant and requires further work-up +/- treatment depending on subtype
Management
Thyroid cancer should be managed by a multi-disciplinary team, including endocrinologists, histopathologists, radiologists, oncologists, and ENT surgeons, alongside specialist nurses and speech and language therapists.
Management varies depending on the cancer subtype, staging, and size. Management options include surgical, chemotherapy, radiotherapy, and radio-iodine therapy, albeit surgery is the primary treatment modality.
Surgical Treatment
- Hemi-thyroidectomy – This involves removing half of the thyroid that contains the lesion, however is only suitable for certain tumours (e.g. small low grade malignancy without extrathyroidal extension or lymph node involvement) or for diagnostic procedures
- Total thyroidectomy – Most malignant disease (tumours ≥4 cm, or with extrathyroidal extension) will require a total thyroidectomy, which involves removing the whole thyroid (including the isthmus); patients will always need to take lifelong thyroid hormone replacement following this surgery
Locally advanced disease may also require neck dissection, to remove groups of lymph nodes from the surrounding region, both to aid diagnosis and attempt to reduce disease spread.
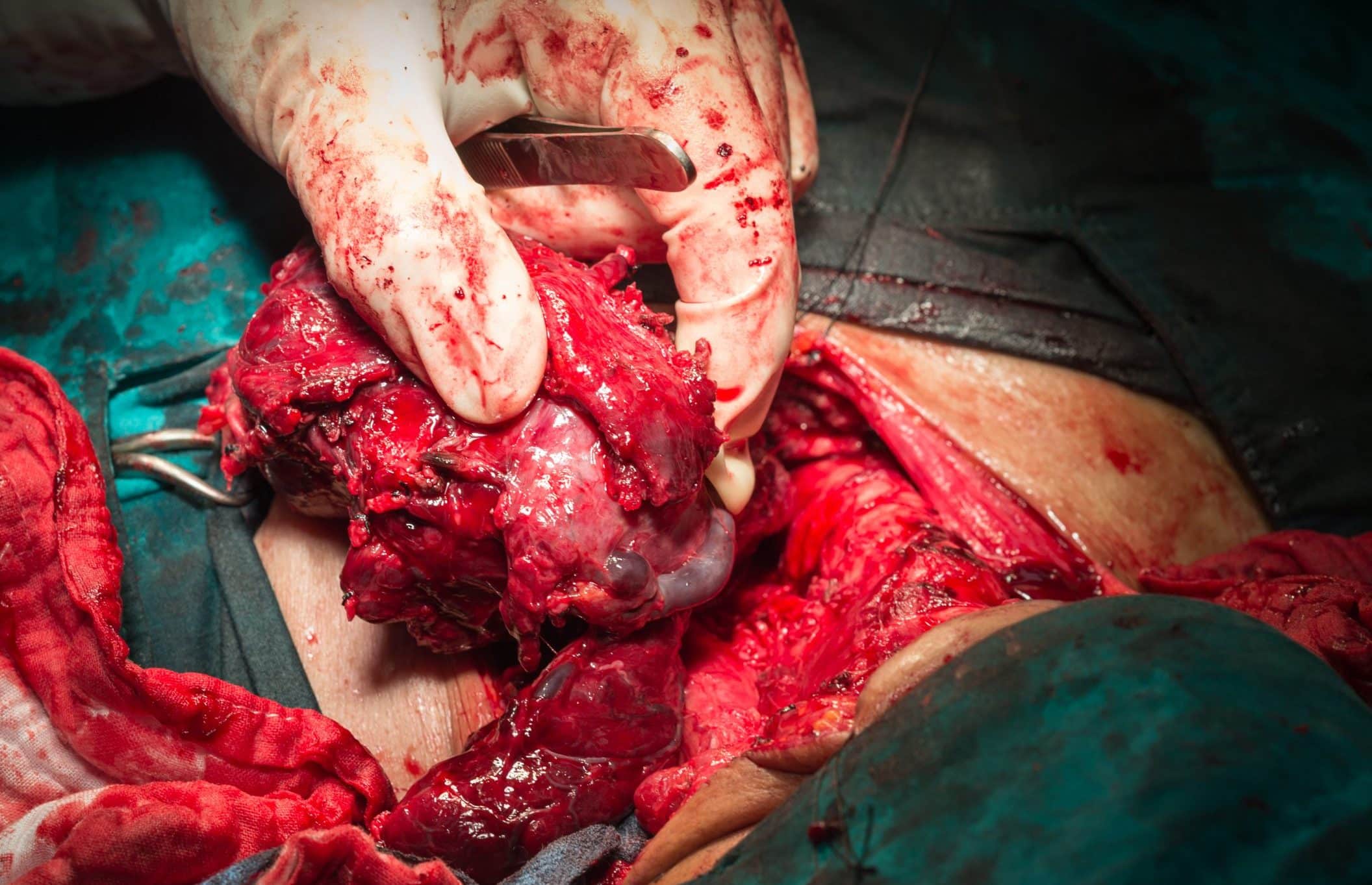
Figure 5 – The thyroid gland, following removal in a total thyroidectomy
Complications of Thyroid Surgery
Bleeding immediately after the operation can result in a haematoma forming beneath the skin. Large haematomas can cause airway obstruction, which is an emergency. In this situation the surgical wound must be re-opened (on the ward!) to allow drainage of the haematoma and the patient will need to go back to theatre to stop the bleeding.
Hypocalcaemia may occur if there is damage to or removal of the parathyroid glands. After a total thyroidectomy, patients must be monitored for clinical features of hypocalcaemia, such as paraesthesia or tetany. PTH and serum calcium levels must be closely monitored (calcium levels can become significantly low within hours post-operatively)
The recurrent laryngeal nerves run close to the thyroid gland, hence care during surgery must to taken to prevent damage causing vocal cord paralysis. Unilateral palsy will result in a hoarse voice however a bilateral paralysis can result in a life-threatening stridor and tracheostomy may be warranted.
Non-Surgical Treatment
Radioiodine therapy involves administration of a radioactive iodine solution, which is taken up preferentially by residual thyroid tissue, acting a focal radiation targeting the malignancy (mainly used for papillary or follicular carcinomas). It is only effective after total thyroidectomy and is used in selective cases who are at higher risk of recurrence (e.g. larger tumours, extrathyroidal extension, lymph node involvement, or incomplete tumor resection).
External beam radiotherapy can be used as primary or adjunct therapy (curative or palliative). Chemotherapy can also be used for similar means, classically lymphomas usually responding well to chemotherapy, and symptoms can improve within a few doses.
Patients should be regularly followed up in the 1st year with serum thyroglobulin levels and ultrasound imaging to monitor for any recurrent disease.
Prognosis
The prognosis of thyroid cancer depends on the histological subtype, the grade, and the stage of the malignancy.
- For papillary cancer, prognosis is quite good with 5-year survival of 98% (this reduced considerably if the tumour has spread beyond the gland)
- Follicular cancer has a high 10-year survival at around 85% (haematogenous spread is a marker of poorer prognosis)
- Medullary cancer also has a good prognosis, with 10-year survival dropping only below 90% when nodal or metastatic spread is seen.
- For anaplastic cancer, there is a very poor prognosis, with a 1-year survival of 10-20%
Key Points
- Thyroid lumps are a common presentation however only a small proportion of them are cancerous
- The main types of thyroid cancer are papillary, follicular, medullary, anaplastic, and lymphoma
- Red flag signs for any thyroid lump include pain, rapid growth, a cough, hoarse voice, or stridor, lymphadenopathy, or tethering of the lump
- Diagnosis is made via Ultrasound Scan followed by Fine Needle Aspiration Cytology
- Management options available range from surgical to medical to palliative