Introduction
Inflammation refers to the initial physiological response to tissue damage, such as that caused by mechanical, thermal, electrical, irradiation, chemical, or infective insults.
It can be acute (lasting for a few days) or chronic (in response to an ongoing and unresolved insult). Inflammation can develop into permanent tissue damage or fibrosis.
Chronic inflammation is an ongoing inflammatory response occurring from an unresolved insult. It results as a continuation of acute inflammation or arising de-novo (whereby the acute inflammatory response has been bypassed).
Inflammatory Cells
Macrophages
Macrophages are the major phagocytic cell in chronic inflammation, acting to engulf and destroy foreign material and/or pathogens, and are derived from monocytes.
Macrophages also act as antigen presenting cells (APCs), whereby antigens are presented from the innate immune cells to the adaptive immune cells. This process allows for a more coordinated and targeted response from the immune system in chronic inflammation. They also secrete growth factors and cytokines, to help coordinate the immune response.
Macrophages can also fuse and form multi-nucleated giant cells (Fig. 1) in chronic inflammation. They are produced in response to certain stimuli, such as a foreign body (foreign-body giant cell), mycobacterium tuberculosis (Langhans giant cell), or fat necrosis (Touton giant cell).
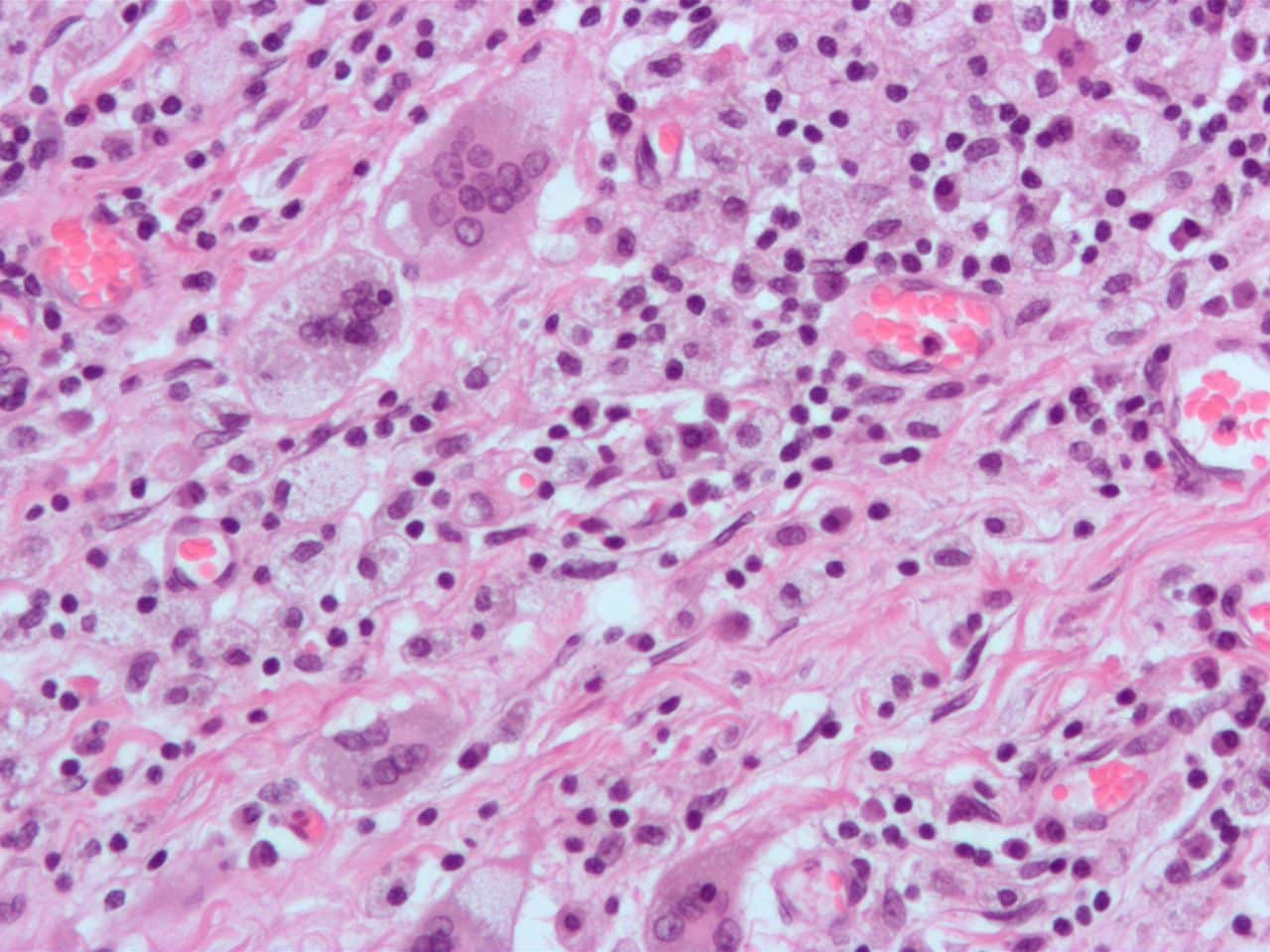
Figure 1 – Multinucleated giant cells, formed by the fusion of macrophages
Lymphocytes
In chronic inflammation, lymphocytes work in conjunction with APCs to process antigens, thereby coordinating a suitable inflammatory response. There are two main types, B lymphocytes and T lymphocytes (Fig. 2).
B Lymphocytes
When appropriately stimulated, B lymphocytes differentiate into plasma cells. Plasma cells are essential for antibody production, which are used for:
- Neutralising microbes and toxins (binding to and blocking the harmful effects of the antigen), to prevent infective and toxic effects of the antigen
- Promote natural killer cells to destroy targeted and tagged pathogens (termed antibody dependant cellular cytotoxicity, or ADCC)
- Facilitate easier phagocytosis by the innate immune cells (termed opsonisation)
T Lymphocytes
T helper lymphocytes (CD4+ cells) act to co-ordinate further targeted inflammatory responses, from both innate and adaptive immune cells. T killer lymphocytes (CD8+ cells) act to co-ordinate the targeted destruction of infected cells.
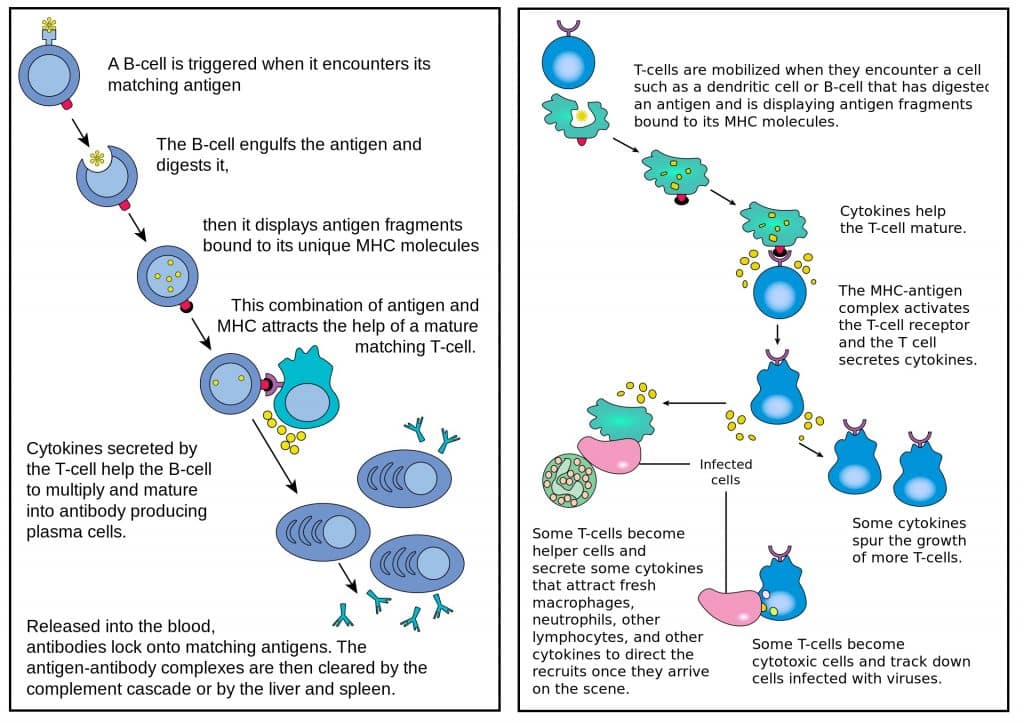
Figure 2 – The roles of B lymphocytes (left) and T lymphocytes (right) in chronic inflammation
Granulomas
In chronic inflammation, macrophages and lymphocytes can combine to form a granuloma (Fig. 3), a means by which the immune system can “wall off” an agent particularly resistant to destruction.
A granuloma contains a collection of elongated macrophages, termed epithelioid cells, surrounding a core of lymphocytes and giant cells attempting to break down the particles.
They are observed in several disease states, such as tuberculosis, sarcoidosis, Crohn’s disease, Rheumatoid arthritis, and Granulomatosis with polyangiitis (GPA).
As granulomatous inflammation progresses, fibroblasts begin to lay down scar tissue, whilst the central core can become necrotic due to the release of enzymes (particularly seen in tuberculosis).
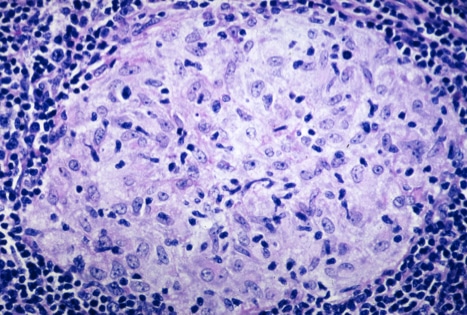
Figure 3 – A granuloma in sarcoidosis, showing a central core of lymphocytes surrounding by macrophages
Key Points
- Chronic inflammation can arise following acute inflammation or de-novo
- The main cells involved are macrophages and lymphocytes
- Macrophages and lymphocytes can combine to form granulomas, acting to “wall off” any agent particularly resistant to destruction
