Introduction
Chronic otitis media (COM) is an inflammatory disorder of the middle ear. It is characterised by persistent or recurrent ear discharge.
Most classifications now separate chronic otitis media into two distinct types:
- Mucosal – occurs due to tympanic membrane perforation and subsequent inflammation of the middle ear mucosa due to infection; it is also known as chronic suppurative otitis media
- Squamous – occurs due to retraction of the tympanic membrane and is associated with the formation of a cholesteatoma
In this article, we shall look at the risk factors, clinical features, and management of chronic mucosal otitis media
Pathophysiology
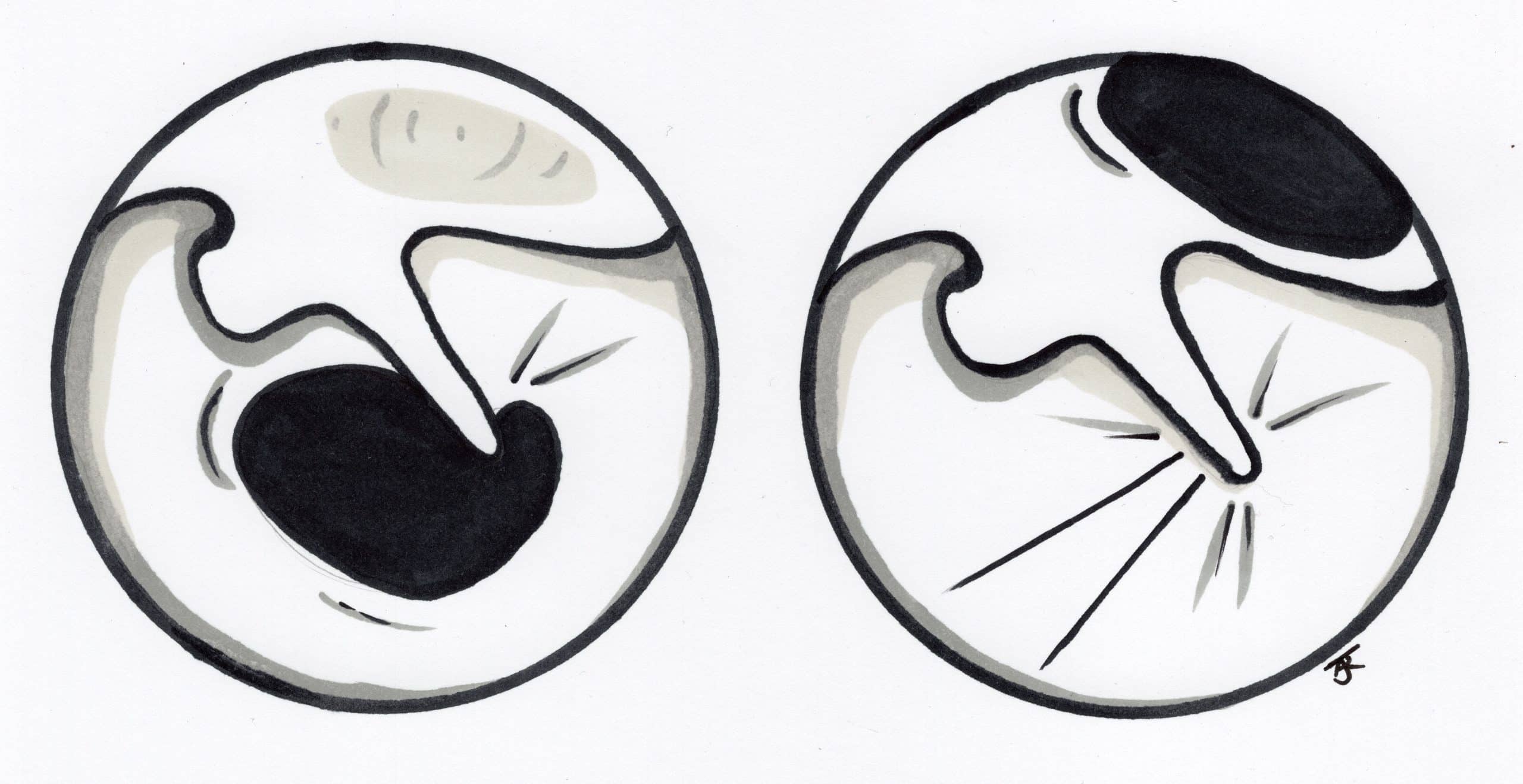
Chronic mucosal otitis media develops due to chronic inflammation of the middle ear mucosa secondary to a perforation in the tympanic membrane as that allows bacteria to enter the sterile middle ear (Fig. 1). The cause of the initial perforation may be infection, iatrogenic (e.g. grommet insertion), or trauma.
Any associated discharge from the perforation is termed an active mucosal COM, also known as “Chronic Suppurative OM” (CSOM). Chronic inactive mucosal COM is equivalent to a chronic dry, perforated tympanic membrane. The mastoid air cells are continuous with the middle ear cavity and may also be affected in this disease, which may result in more significant otorrhoea.
Chronic mucosal otitis media is a common condition. It has a prevalence of 0.9% amongst children and 0.5% amongst adults in the UK. Half of all cases develop a degree of hearing impairment.
Aetiology
Recurrent acute otitis media is the most common cause of mucosal chronic otitis media. Other associated risk factors include previous traumatic perforation of the TM, insertion of grommets, and craniofacial abnormalities.
Clinical Features
Patients will present with a chronically discharging ear (by definition this should be for >6 weeks), in the absence of fever or otalgia. If fever or pain is present then other diagnoses should be considered, such as otitis externa, mastoiditis, or intracranial involvement.
On examination, there will be a perforation in the tympanic membrane visible on otoscopy (Fig. 2). Patients will often have a history of recurrent AOM, previous ear surgery, or trauma to the ear.
It is important to test facial nerve function and document this clearly. Hearing loss can occur, which is nearly always conductive hearing loss (unless the disease is extensive)
Investigations
Audiograms and tympanometry should be performed in suspected cases, although this may not be appropriate in a heavily discharging ear. Microbiological swabs for culture and antibiotic sensitivities are useful (especially when initial treatment options fail).
Whilst the diagnosis of chronic mucosal otitis media is made clinically, any suspicion of cholesteatoma warrants a CT scan of the petrous temporal bone for further assessment.
Referred Ear Pain
If the external ear canal and drum are normal, with normal pneumatic speculum, pain is not from ear disease but instead referred pain. Conditions to consider, due to the external ear’s numerous innervations, include:
- CN V = Parotid gland, upper molar teeth, or TMJ pathology
- CN VII = Ramsey Hunt syndrome
- CN IX and CN X = Malignancy of the posterior ⅓ tongue, piriform fossa, larynx, or infective causes, such as tonsillitis or quinsy
Management
The mainstay of treatment in chronic mucosal otitis media is aural toileting and topical/oral antibiotic or steroid treatments until symptoms reduce or resolve. It is also very important to tell the patients to keep the ear dry and clean.
Most tympanic membrane perforations will heal spontaneously however large perforations can persist and referral for surgical management may be required, if there is significant conductive hearing loss or recurrent acute otitis media.
Surgical Management
The aim of surgical management is to close the perforation in the tympanic membrane, thereby relieving the symptoms of persistent discharge and preventing recurrent infection.
Surgery can also potentially improve hearing, although this will largely depend on the pre-operative state of the auditory apparatus.
Surgical options include:
- Myringoplasty – closure of perforation in pars tensa
- The closure is achieved by patching on an autologous graft, usually harvested from the tragal cartilage or temporalis fascia
- Tympanoplasty – a myringoplasty combined with reconstruction of the ossicular chain
Key Points
- Mucosal COM is caused by chronic inflammation secondary to a perforation in the tympanic membrane
- Patients will present with a chronically discharging ear, in the absence of fever or otalgia
- The mainstay of treatment is aural toileting and topical antibiotic/steroid treatments until symptoms reduce or resolve
- Surgical options include myringoplasty or tympanoplasty