Introduction
- Introduce yourself to the patient
- Wash your hands
- Explain the examination to the patient
- Reassure them that you will stop if it becomes too painful at any point
- Ensure verbal consent is adequately obtained
- Offer the patient a chaperone if required
Always work through a structured approach as below unless instructed otherwise; be prepared to be instructed to move on quickly to certain sections by any examiner.
Inspection
Assess the external genitalia and groin for:
- Obvious skin changes, ulcers, warts, or chancres, bruising
- Scars (including circumcision)
- Penile anatomy, specifically any hypospadias, phimosis, or paraphimosis
- Check for evidence of any penile discharge, if relevant
- Swellings or lumps in the groin
Then inspect the scrotum for:
- Any scars* or skin changes
- Typically incisions are made on the midline raphe, however small bilateral incisions are often used for bilateral vasectomy
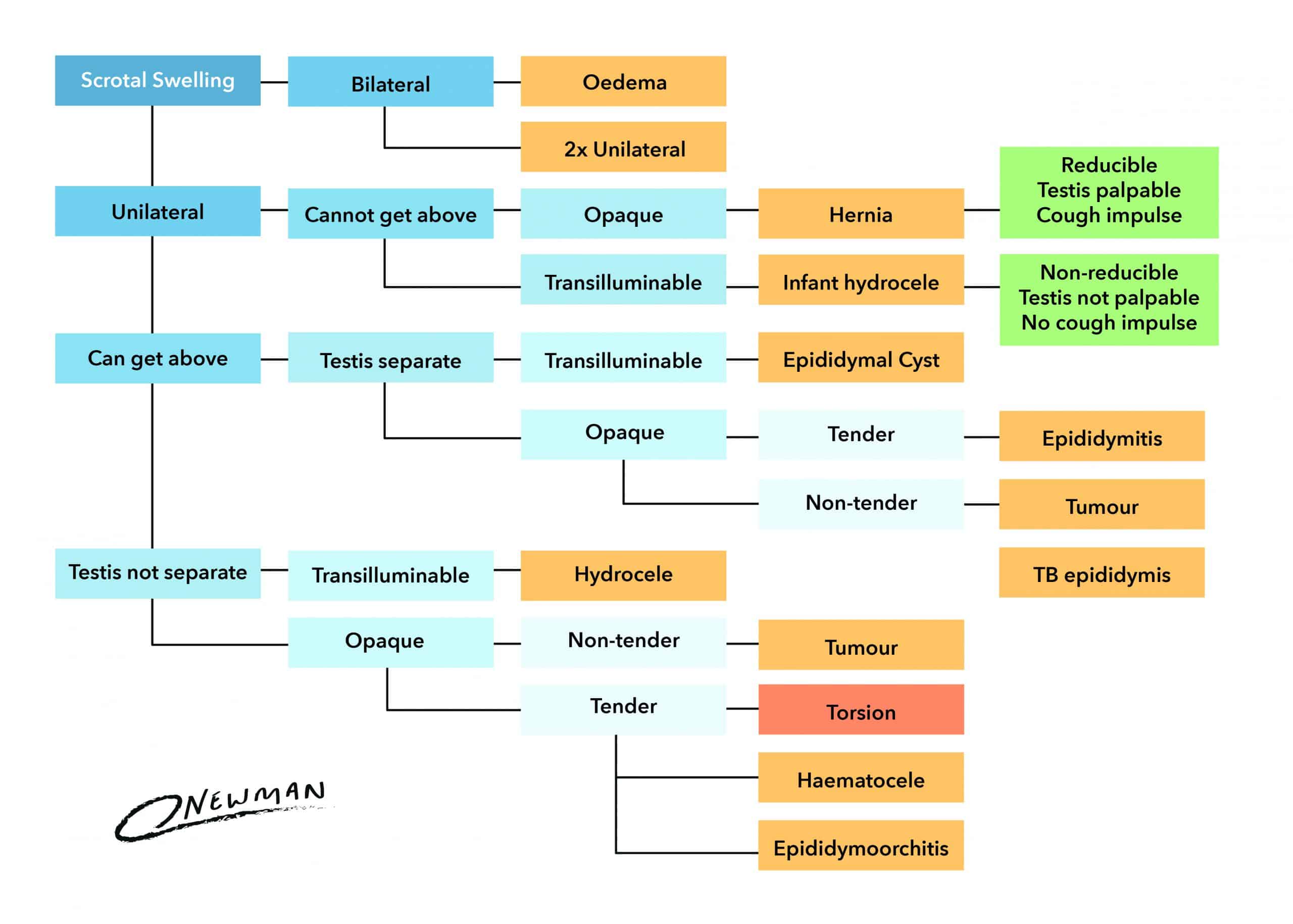
- Swelling, either unilateral or bilateral
- Asymmetry between the testes, specifically noting the size & positioning (such as high riding or undescended)
*Remember that an orchidectomy for suspected testicular cancer will be performed via an inguinal incision, therefore the scar may be in the groin
Palpation
- Before palpating, assess for the cremasteric reflex bilaterally (see Appendix)
- Palpate the scrotum gently using both hands, checking that both testes are present within the scrotum.
- If you are unable to find both testes, check the inguinal canal and perineum for an undescended or palpable ectopic testis
- Palpate each testis individually*, using the index finger and thumb to palpate the body of the testis. Check for the size and consistency of each testis, feeling for any lumps or irregularities. Repeat for the other testis.
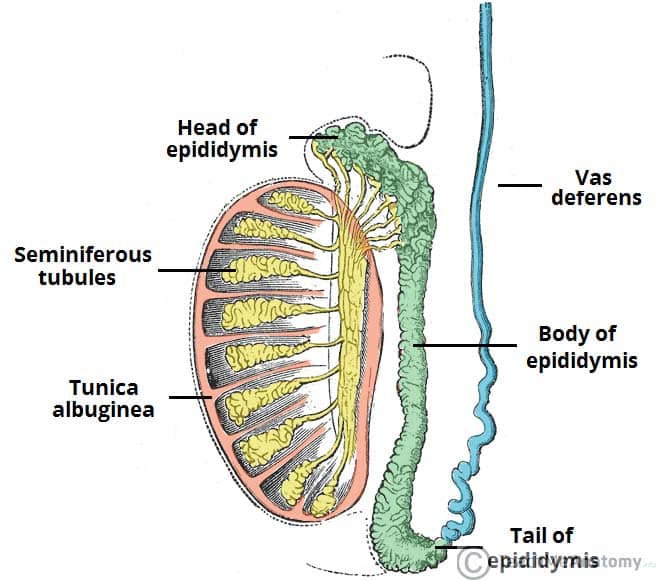
- Palpate the epididymis, located at the posterior aspect of the testicle (only the head of the epididymis can typically be palpated)
- Palpate the spermatic cord, by gently pulling down the testis and placing your index finger and thumb on the neck of the scrotum.
*If there are concerns about one testis, start with the “normal’”testis and then proceed to the other testis
Completing the Examination
Remember, if you have forgotten something important, you can go back and complete this.
To finish the examination, stand back from the patient and state to the examiner that to complete your examination, you would like to perform a full abdominal examination
Appendix
The Cremasteric Reflex
The cremasteric reflex is produced by the genitofemoral nerve (L1) when the inner part of the thigh is touched. This stimuli causes the cremaster muscle, which is located in the inguinal canal and scrotum surrounding the testis and spermatic cord, to contract.
When the cremaster muscle contracts, it draws the testis up towards the inguinal canal and out of the scrotum. Loss of the cremasteric reflex is associated with testicular torsion, but always consider the clinical picture (plus any Doppler imaging) in addition to this clinical sign.
Prehn’s Sign
Prehn’s Sign can be used to help differentiate between acute epididymitis and testicular torsion in those presenting with testicular pain. The sign is elicited by the patient lying supine on the bed and the scrotum is then elevated by the examiner
A negative Prehn’s sign is when there is no pain relief on lifting the affected testicle (more suggestive of testicular torsion), whilst a positive Prehn’s sign is when there is pain relief on lifting the affected testicle (more suggestive of epididymitis).