Introduction
An aneurysm is defined as a persistent, abnormal dilatation of an artery above 1.5 times its normal diameter. The abdominal aorta is the most commonly affected vessel, but peripheral artery aneurysms and visceral artery aneurysms can also occur.
Broadly speaking, the presentation of these aneurysms will be either asymptomatic (found incidentally), symptomatic but not ruptured, or symptomatic secondary to a rupture (stable or unstable)
Risk Factors
The aetiology of peripheral and visceral aneurysm is largely unknown. Possible causes include trauma, infection, connective tissue disease (e.g. Marfan’s disease), or inflammatory disease (e.g. Takayasu’s aortitis).
Risk factors for such aneurysms include smoking, hypertension, hyperlipidaemia, and family history.
Management
Peripheral and visceral aneurysms are usually best investigated with CT angiography. MR angiography is a good alternative, mainly due to the reduced radiation exposure, particularly for younger patients who may require long follow up. Ultrasound duplex scans can be useful for detection and follow up, however further anatomical information gleaned from cross sectional imaging will be required to help with planning of treatment.
Management will usually involve either watchful waiting whilst optimising medical therapy, such as antiplatelet and statin therapy +/- smoking cessation, or surgical intervention (endovascular or open), depending on the location and size, as well as associated symptoms.
This article will focus on the more common types of peripheral and visceral aneurysms, including their presentation, investigations needed, and potential management.
Peripheral Artery Aneurysms
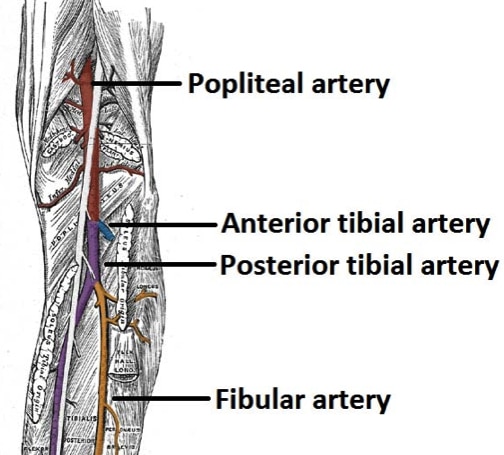
The most common peripheral artery aneurysms occur in the popliteal artery and femoral artery.
Popliteal Artery
Popliteal aneurysms are the most common site for peripheral aneurysms, accounting for 70-80%. They have a high risk of embolisation and/or occlusion.
Presentation
Popliteal aneurysms will usually present symptomatically as either acute limb ischaemia (from aneurysm thrombosis or distal emboli) or less commonly with intermittent claudication. Thrombosis of a popliteal aneurysm has a 50% amputation rate due to trash to the tibial vessels.
Alternatively, they may be found incidentally, such as in patients being worked up for AAA repair or awaiting knee replacement, or from compression symptoms on the popliteal vein or peroneal nerve. The rupture of popliteal artery aneurysms is rare.
Investigation
The initial investigation for a suspected popliteal aneurysm is an ultrasound duplex scan, as this will allow the differentiation between other causes of a popliteal fossa swelling, such as a Bakers cyst or lymphadenopathy, whilst also looking for signs of aneurysm thrombosis and embolisation into the tibial vessels.
Further imaging will often be via CT Angiogram or MR Angiogram. These imaging modalities allow good anatomical assessment of the aneurysm (useful for operative planning) and in the assessment of distal arteries to assess patency.
Management
Due to risk of embolic events, symptomatic popliteal aneurysms should be treated regardless of their size; if distal embolisation is seen on imaging, this should warrant treatment at an early stage.
If asymptomatic but greater than around 2.5cm, most should be considered for treatment. Those with a large thrombus load should also have a low threshold for treatment and can be treated at 2.0cm.
In cases of thrombosis, if there is no patient tibial vessel then embolectomy or thrombolysis can be attempted to improve run off prior to/at the time of bypass surgery.
Surgical Intervention
Both open and endovascular options are available for treatment of popliteal aneurysms.
- Endovascular repair involves stent insertion across the aneurysm and requires a normal calibre artery above and below the aneurysm for the stent to seal in
- This procedure does incur risks of continued aneurysm sac filling through collateral vessels and in-stent thrombosis can occur; it is done under local anaesthetic and is often the preferred choice in unfit patients
- Surgical repair involves ligation of the aneurysm or resection of the aneurysm with a bypass graft (either a vein from the patient (preferred) or a graft)
- This can be in the form of an above to below knee popliteal bypass, or through a posterior approach to the knee, opening the aneurysm sac then inserting a tube graft from top to bottom (this approach is often done using prosthetic)
Femoral Artery
Femoral artery aneurysms are typically pseudoaneurysms, with the two major causes being:
- Percutaneous vascular interventions
- Patient self-injecting, typically intravenous drug users (IVDU) who inject into their groin
Presentation
The clinical features from a femoral artery aneurysm are from either thrombosis, rupture, or embolisation of the aneurysm. In IVDU cases, concurrent infection may also be present.
As a consequence, patients will present with varying degrees of claudication or acute limb ischaemia, but often with no symptoms other than a swelling in the groin.
Investigation and Management
These aneurysms should be investigated initially with ultrasound duplex scan, before requiring CT Angiography or MR Angiography for further anatomical imaging and operative planning.
The mainstay of treatment for femoral aneurysms is open surgical repair (endovascular repair is rarely performed for such a pathology).
Visceral Artery Aneurysms
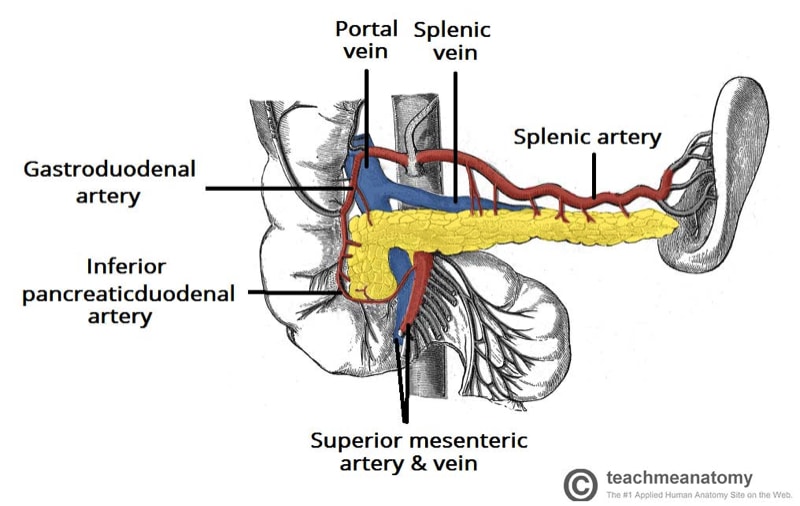
The visceral arteries most commonly affected by aneurysm formation are the splenic artery, hepatic artery, and renal artery.
Splenic Artery
Splenic artery aneurysms are the most common type of visceral aneurysm, comprising around 60% of the total.
The main risk factors for their development are female sex, multiple pregnancies, portal hypertension, and pancreatitis or pancreatic pseudocyst formation.
Presentation
Those that are symptomatic will present with a vague epigastric or left upper quadrant abdominal pain. Those that rupture will present with severe abdominal pain and haemodynamic compromise.
Investigation and Management
The mainstay of investigation for splenic artery aneurysms is by CT Angiography or MR Angiography. Ultrasound imaging can sometimes be used for monitoring (albeit only in thinner patients).
First line management option is endovascular repair; this is best done with embolisation or covered stent grafts, once the patient is haemodynamically stable (an open repair may be advised in the unstable patient which would entail ligation of the aneurysm and bypass).
Hepatic Artery
Hepatic artery aneurysms are the second most common of the visceral aneurysms, accounting for around 20% of cases.
Percutaneous instrumentation is associated in 50% of cases, yet the remainder of cases may be from trauma, degenerative disease, or post-liver transplant (false aneurysms forming around vessel anastomoses).
Presentation
Most cases are usually asymptomatic, yet stable symptomatic cases can often present with vague RUQ or epigastric pain; jaundice can less commonly occur if there is any biliary obstruction.
Investigation and Management
Much like splenic aneurysms, the mainstay of investigation for hepatic artery aneurysms is by CT Angiography or MR Angiography.
First line management is endovascular repair; this is best done with embolisation or covered stent grafts, once the patient is haemodynamically stable, in those with suitable anatomy (an open repair may be advised in the unstable patient or with unsuitable anatomy).
Renal Artery
A renal artery aneurysm is often found incidentally and is asymptomatic. However, in symptomatic cases, patients may present with haematuria, resistant hypertension, or loin pain (including those with renal infarction).
Investigation and Management
Renal artery aneurysms should also be investigated by CT Angiography or MR Angiography.
Mainstay of treatment is via endovascular repair. A stent can be inserted easily if the aneurysm is affecting the main renal artery, otherwise if it is affecting the hilum, endovascular repair with coils and covered stent graft may be used.
An alternative option, albeit rarely done, is to explant the kidney and perform a renal transplant.
Key Points
- The aetiology of most peripheral and visceral aneurysms is largely unknown
- The most common clinical presentation is being found incidentally on routine imaging
- Peripheral and visceral aneurysms are usually best investigated with CT angiography
- Management is chosen predominantly on a case-by-case basis, however the surgical treatments offered are often a choice between endovascular repair or open repair