This article is for educational purposes only. It should not be used as a template for consenting patients. The person obtaining consent should have clear knowledge of the procedure and the potential risks and complications. Always refer to your local or national guidelines, and the applicable and appropriate law in your jurisdiction governing patient consent.
Overview of Procedure
A parotidectomy is an operation performed to surgically remove one of two parotid glands, which are the largest major salivary glands. It is performed for parotid gland tumours; most (80-85%) are benign with a small risk for malignant conversion and a minority (15-20%) are malignant.
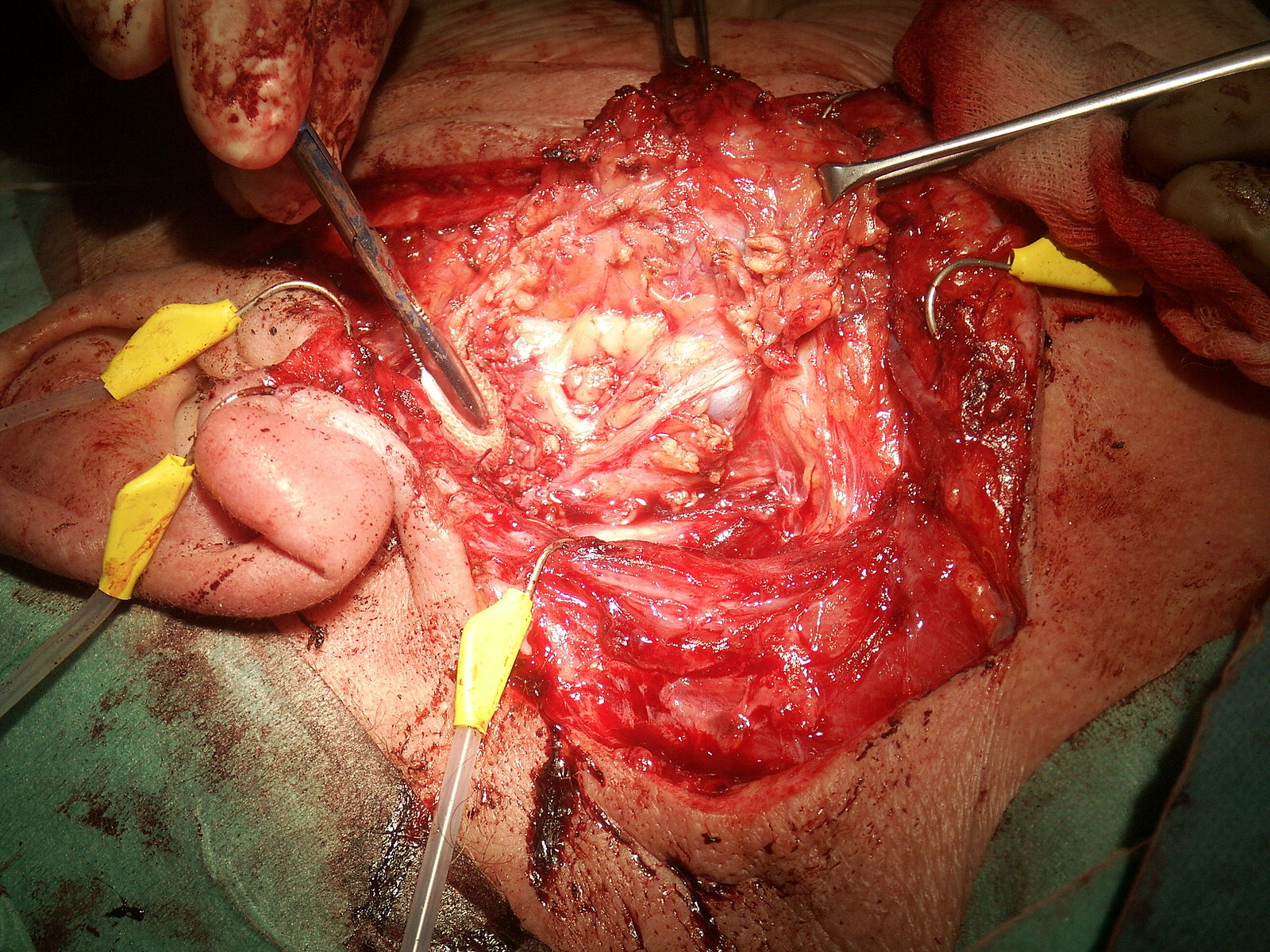
The operation is performed under general anaesthesia. A long incision is made anterior to the tragus down down to the neck below the mandible (known as a Modified Blairs incision). A subplatysmal flap is raised and careful dissection of the parotid gland is performed (Fig. 1).
Parotidectomies may only remove the superficial lobe, however If there is significant invasive disease then a total parotidectomy may be performed (i.e. superficial and deep lobes); this poses much higher risk of facial nerve injury.
Complications
Intraoperative
| Complication | Description of Complication | Potential Ways to Reduce Risk |
| Haemorrhage | Potential for injury to the branches of the carotid artery or external jugular vein | Adequate haemostasis and careful dissection throughout the procedure |
| Anaesthetic Risk | Includes damage to the teeth, throat and larynx, reaction to medications, nausea and vomiting, cardiovascular and respiratory complications | Forms a part of the anaesthetist assessment before the operation |
Early
| Complication | Description of Complication | Potential Ways to Reduce Risk |
| Pain | Use of regular analgesia to reduce pain post-operatively | |
| Infection | Use of meticulous aseptic technique throughout and antibiotic prophylaxis if required | |
| Facial Nerve or Greater Auricular Nerve injury | Extracranial branches of the facial nerve or greater auricular nerve can be temporarily (neuropraxia) or permanently (neurotmesis) injured | Careful dissection technique to ensure no injury to nerve and minimising use of thermal energy near nerves |
| Haematoma | Placement of a drain intraoperatively and ensuring adequate haemostasis at the end of the operation (use of Valsalva to identify any bleeding vessels before closure) | |
| Seroma | A build of a serous fluid in an area the space created following removal of tissue | Suture closure of the dead space intra-operatively |
| Salivoma or parotid fistula | An abnormal communication forms between the skin and the salivary duct or gland, through which saliva is discharged |
Late
| Complication | Description of Complication | Potential Ways to Reduce Risk |
| Cosmetic problems | A concavity may be noticeable after the procedure due to resection of the parotid tissue, alongside the scar formation | |
| Frey’s syndrome | Disruption of local parasympathetic nerve fibres, which can result in gustatory sweating | |
| Disease recurrence | Achieve good clear resection margins intra-operatively |