Introduction
Phalangeal fractures are a common presentation to the emergency department, accounting for around 10% of all bony fractures. They are more common in males and the distal phalanx is most commonly injured.
Phalangeal fractures can occur through crush, axial loading, torsional, or hyperflexion* mechanisms. Sports injuries and machinery accidents are the most common causes of phalangeal injuries, especially in younger patients, with falls being the more common cause in older patients.
While open operative approaches have been popular previously, non-operative or minimally-invasive percutaneous interventions have proved increasing popular management options in recent years. Management decisions need to balance between “overtreatment” leading to stiffness versus “undertreatment” leading to deformity.
*Tendon avulsion injuries, e.g. Mallet finger, from forced extension can lead to phalangeal fractures, as well as hyperextension injuries at the PIPJ with avulsion fractures linked to the volar plate ligament
Clinical Features
Patients with phalangeal fractures usually present with a history of trauma, even from potentially a minor impact. Patients will report localised pain at the affected area, with reduced function of the affected digit.
Further factors of the history are essential for decision making include time and mechanism of injury, patient age, hand dominance, occupation, tetanus status, and co-morbidities
On examination, there may be an obvious deformity, with tenderness and/or reduced movement at the affected site. There can be concomitant joint subluxation, joint ligament injury, or tendon avulsion (mainly in mallet injuries), or nail bed injuries (in distal phalangeal fractures).
Assess (and document) the digit’s neurovascular status, as digital vessel and nerve injuries are commonplace. Ensure to check for signs of open fractures.
The most important aspect of the examination is checking function*, as this will guide whether non-operative treatment is feasible.
*Ask the patient to flex and extend the digit (as pain / swelling allows) and assess for scissoring and rotation on flexion, and check the stability of the joints (to check for ligamentous injury).
Differential Diagnosis
Any patient presenting following trauma with pain and tenderness of a digit may have an isolated tendon injury (e.g. FDP tendon or ED tendon), a MCPJ or IPJ dislocation, a ligament injury, or soft tissue mass (e.g. ganglion, osteoarthritis, or rheumatoid arthritis)
Investigations
The mainstay of initial assessment for any suspected phalangeal fracture is through plain film radiographs (Fig. 2); this should be in the view antero-posterior, lateral, and oblique.
Further CT imaging may be required for complex intra-articular fractures, which can aid in operative planning. If any concurrent ligamentous avulsion is suspected, MRI imaging may be required.
Management
An A to E assessment is vital for any patient presenting following trauma, stabilising the patient and prioritising more serious injuries first. Once the patient is stable, any suspected phalangeal injuries can then be focused on during the secondary survey; ensure to check and document the neurovascular status.
Definitive management* focuses around ensuring adequate bony alignment and stabilisation, with early mobilisation to ensure optional functional outcomes. As such, any significantly displaced fracture should initially be reduced in A&E, with sufficient analgesia.
Non-operative management can be trialled in certain phalangeal fractures, whereby following an initial period of immobilisation (through splinting or “buddy taping”), intensive period of rehabilitation with a hand therapist is required. Early mobilisation aids to reduce any potential complications of a surgical approach, such as infection, stiffness, metalwork removal, or secondary tenodesis.
*All open fractures proximal to the distal phalanx usually need formal debridement and washout in theatre
Surgical Management
The decision for surgery depends on many different patient and fracture factors.
The main indications for operative management for phalangeal fractures are those that are unstable, open, or comminuted. Those that have concomitant associated soft tissue injury, or significant angulation or shortening will often require an operation too.
Operative management involves either open reduction with internal fixation (ORIF) or closed reduction percutaneous pinning (CRPP) using K-wires. External fixators are rarely used in complex fracture patterns, where internal fixation is impossible.
Distal phalangeal fractures can be associated with nailbed injuries or tendon avulsion injuries, which would also require repair.
Complications
Common complications include stiffness, due to prolonged immobilisation, malunion, or non-union, are uncommon. Post-operative complications, for those that undergo surgical management, include metalwork infection, pain, scarring, and tendon adhesions.
Phalangeal Dislocation
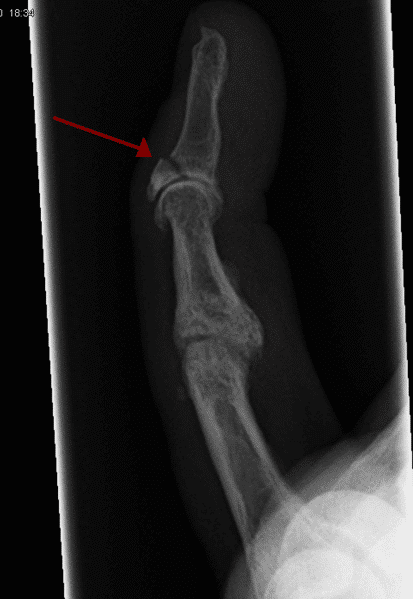
Phalangeal dislocations are less common that phalangeal fractures. They can be either at the PIPJ (more common), DIPJ (often associated with tendon avulsion), or the MCPJ, more common in the dorsal direction secondary to a hyperextension injury (Fig. 3).
Dislocations will also be diagnosed through plain film radiographs (antero-posterior, lateral, and oblique views).
Management of a simple dislocation is generally via closed reduction and splinting/buddy-taping. If closed reduction is not possible, the joint will be opened and reduced in theatre, termed an “open reduction”; if it is still unstable in theatre, the joint (along with any fracture present) can be fixed with a temporary K-wires.
Prognosis of phalangeal dislocations are generally good, if a stable reduction can be achieved. Complications include stiffness, pain, and recurrence.
Key Points
- Phalangeal fractures are a common presentation to the emergency department
- Patients with phalangeal fractures usually present with a history of trauma, reporting localised pain at the affected area and reduced function of the affected digit
- The mainstay of initial assessment for any suspected phalangeal fracture is through plain film radiographs
- Non-operative or minimally-invasive percutaneous interventions have proved increasing popular management options in recent years