This article is for educational purposes only. It should not be used as a template for consenting patients. The person obtaining consent should have clear knowledge of the procedure and the potential risks and complications. Always refer to your local or national guidelines, and the applicable and appropriate law in your jurisdiction governing patient consent.
Overview of Procedure
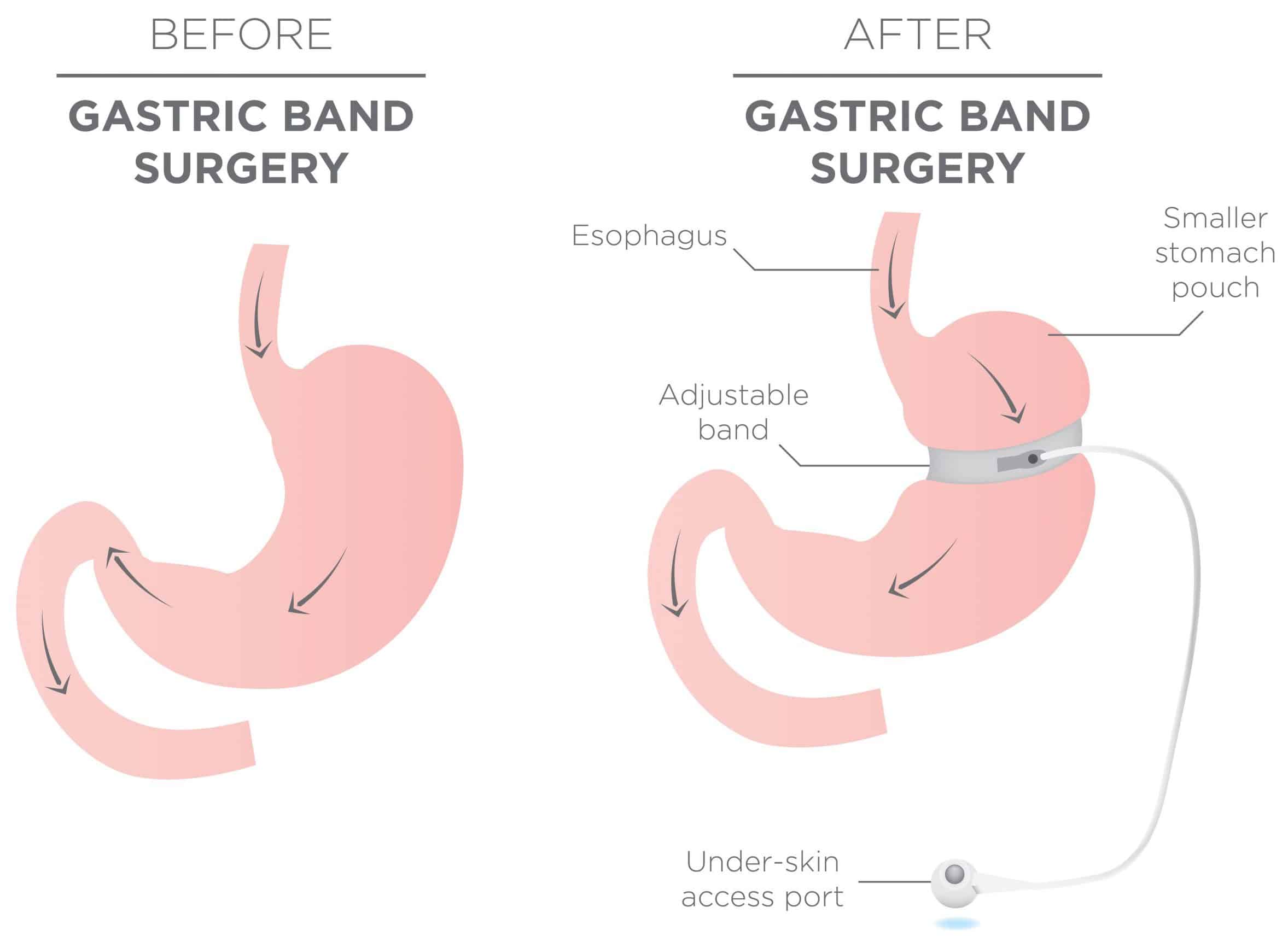
A gastric band procedure primarily works via a restrictive mechanism. The pars lucida and greater omentum are dissected and a restrictive band is placed around the stomach, and is a core procedure within bariatric surgery.
It is usually performed as day-case procedure. It is a lesser physiological insult than the other bariatric operations, and so is typically viewed as having fewer initial complications.
However, the degree of weight loss generated is believed to be less and a substantial proportion of patients develop band slippage or erosion, and may require further surgery (either band removal or conversion to sleeve / bypass).
Complications
Intra-Operative
| Complication | Description of Complication | Potential Ways to Reduce Risk |
| Haemorrhage | Damage to any of the surrounding structures can cause significant haemorrhage | |
| Injury to surrounding structures including bowel, liver, and spleen | Damage can occur to any surrounding organ during the surgery | |
| Anaesthetic risks | Includes damage to the teeth, throat and larynx, reaction to medications, nausea and vomiting, cardiovascular and respiratory complications | Forms a part of the anaesthetist assessment before the operation |
Early
| Complication | Description of Complication | Potential Ways to Reduce Risk |
| Infection | Includes both wound infections and intra-abdominal collections, as well as respiratory or urinary tract infections post-operatively | Intravenous antibiotics at induction, wound irrigation at closure, and early mobilisation |
| DVT or PE, MI, Stroke, or Mortality | As with any major surgery, whilst these events are uncommon, important to be aware of; the mortality risk is over 1 in 200 | Adequate pre-optimisation and anaesthetic assessment, peri-operative prophylactic LMWH, high-dependency level care post-operatively |
Late
| Complication | Description of Complication | Potential Ways to Reduce Risk |
| Metabolic and endocrine disturbances | Changes to absorption and gastric secretions of the alimentary canal can affect nutrition considerably post-operatively, although these are less than compared to other bariatric procedures | The involvement of a specialist bariatric dietician in the management of bariatric patients is essential |
| Failure to lose weight | Gastric band may not be effective in all patients and subsequent alternative bariatric procedures may be required | |
| Band slippage | If the band position slips, this can become a surgical emergency, as this can lead to ischaemia of the stomach; this often requires urgent surgical removal of the band | |
| Band erosion | The band can erode into the stomach; treatment can involve laparoscopic excision of the band, or even laparotomy +/- partial gastrectomy | |
| Oesophageal dilatation | This occurs due to over-eating and the oesophagus becomes dilated above the restriction; this can lead to oesophageal dysmotility and dysphagia, requiring band deflation or removal | |
| Injection port infection | As with any foreign body, the tube and port can become infected |