This article is for educational purposes only. It should not be used as a template for consenting patients. The person obtaining consent should have clear knowledge of the procedure and the potential risks and complications. Always refer to your local or national guidelines, and the applicable and appropriate law in your jurisdiction governing patient consent.
Overview of Procedure
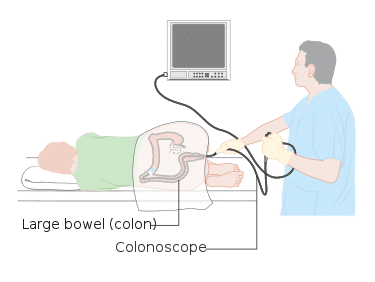
This procedure involves insertion of an endoscope through the anal canal into the large intestine, either to the distal transverse colon (in flexible sigmoidoscopy) or the ileocaecal junction (in colonoscopy).
The aim is to assess the bowel for a variety of pathologies, such as malignancy, inflammatory bowel disease, or diverticular disease. Biopsies can be taken if required. Most centres will require bowel preparation pre-operatively, yet this can vary between units.
Complications
Intra-Operative
| Complication | Description of Complication | Potential Ways to Reduce Risk |
| Haemorrhage | Damage to the bowel may cause significant bleeding, as well as any biopsy sites, for up to 2 weeks. | |
| Perforation | Perforation of the bowel is a rare (1 in 1000) but serious complication. | |
| Sedation Risks | Sedatives, such as midazolam, are often used yet can depress the cardio-respiratory system. | Always use monitoring and beware of using sedation in frail patients with co-existing cardio-respiratory disease or morbid obesity |