Introduction
Sudden sensorineural hearing loss (SSNHL), also known as idiopathic sensorineural hearing loss, is a common presentation to ENT services.
For patients presenting with sudden onset hearing loss, SSNHL is a diagnosis of exclusion, as other more important differentials must be excluded first prior to SSNHL being diagnosed. The majority of cases are unilateral, with around half of patients experiencing full restoration of hearing with 2 weeks.
It has a prevalence of around 5 to 27 patients per 100,000, with the condition more likely to develop in those of increasing age. Other risk factors for its development are smoking and hypertension.
The aetiology for SSNHL is unclear, however current hypotheses for its development include either viral infection (i.e. viral neuronitis), a vascular impairment, or as an autoimmune disorder.
Clinical Features
Patients with SSNHL with present with acute onset of sensorineural hearing loss*, developing within 72hrs. This is often associated with tinnitus and vertigo.
Importantly, there is an absence of otorrhoea, otalgia, or focal neurological defects (all of which would suggest alternative diagnoses), as well as no obvious precipitants, such as recent head trauma or surgery.
Ensure to perform both an ear examination, including Rinne’s and Weber’s test, and neurological examinations.
*Specifically, this must be a sensorineural loss of worse than 30db across three consecutive frequencies on pure tone audiometry
Differential Diagnoses
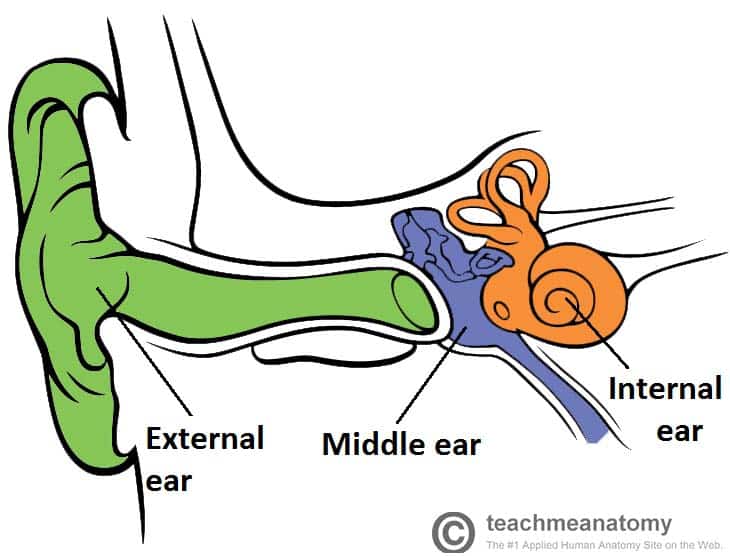
Ensure to differentiate between a conductive and sensorineural hearing loss, as this will help focus differentials.
For a sudden-onset sensorineural hearing loss, differentials include acoustic neuroma, ischaemic or haemorrhagic stroke, or multiple sclerosis.
Investigations
All patients presenting with acute sensorineural hearing loss should undergo Pure Tone Audiometry (PTA) and Tympanometry (Fig. 2).
Depending on the presentation, patients should then undergo urgent blood tests, including Full Blood Count, Erythrocyte Sedimentation Rate (ESR), Autoantibody Screen, Coagulation Screen, and Syphilis serology
An urgent outpatient MRI scan of the internal auditory meatus should be performed, to assess for the presence of acoustic neuroma.
Management
SSNHL should be viewed as an otological emergency, with prompt treatment aimed at minimising long term hearing loss, to help improve quality of life and reduce functional impairment.
The mainstay of treatment is with oral steroid therapy. This is often via a weaning regime, given alongside a proton pump inhibitor, over the course of several weeks; the efficacy of treatment is reduced if treatment is delayed, especially after 2 weeks from presentation.
Following steroid treatment, patients should return for repeat clinical review and repeat PTA. Should there be minimal or no improvement, salvage intratympanic steroids can be considered.
In cases of ongoing hearing loss, referral to audiology for hearing aids fitting (Fig. 3), and ensure adequate psychological support provided.

Figure 3 – Fitting of a hearing aid on a patient with hearing loss
Key Points
- Diagnosis of sudden sensorineural hearing loss (SSNHL) requires ruling out important differentials such as stroke, infection, or autoimmune pathology
- All patients with suspected SSNHL should undergo Pure Tone Audiometry and Tympanometry
- The mainstay of treatment is with oral steroid therapy
- Early presentation and initiation of treatment is essential to improve patient outcomes