Introduction
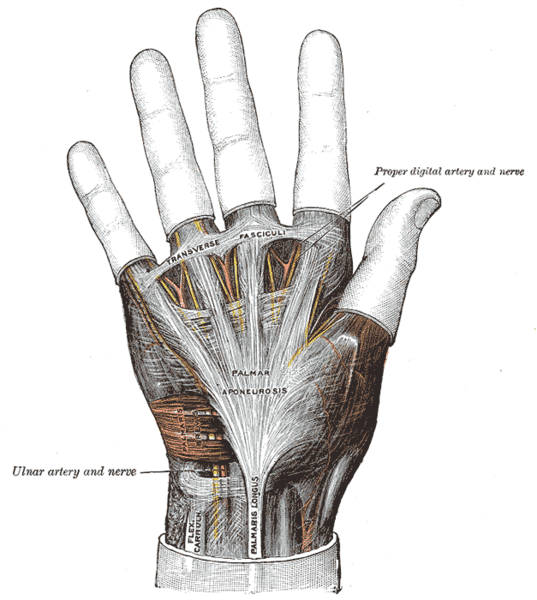
A Dupuytren’s contracture is a common condition involving contraction of the longitudinal palmar fascia.
Typically starting as painless nodules, fibrous cords develop at the metacarpophalangeal (MCP) and interphalangeal (IP) joints, which can severely limit digital movement. This in turn can significantly reduce patient quality of life.
The condition is around six times more common in men, with peak onset in those aged 40-60yrs. It most commonly affects the ulnar digits (ring and little finger).
Pathophysiology
Dupuytren’s contracture involves the proliferation of myofibroblasts and alteration of the collagen matrix of the palmar fascia. This compositional change leads to a thickening and contraction of the palmar fascia*.
The disease progresses in a stepwise pattern, although the rate that it does this is variable:
- Pitting and thickening of the palmar skin and underlying subcutaneous tissue, with a loss of mobility of overlying skin
- Firm painless nodule(s) begins to form, becoming fixed to the skin and the deeper fascia, gradually increasing in size
- A cord develops in the affected area, which begins to contract over months to years
- Contraction of the cord flexes the MCP and proximal IP joints, leading to progressive flexion deformity in the fingers
Whilst the condition is considered idiopathic, there are associations to certain genetic and environmental factors in the disease process.
*Similar clinical conditions have also been described that involve thickening of fascia in other body areas, such as Leddarhose disease (plantar fibromatosis), Peyronie disease (penile fibromotosis), and Garrod nodes (fibromotosis of dorsal proximal interphalangeal joints)
Risk Factors
The main risk factors for the condition include smoking (up to 3 times more common in smokers), alcoholic liver cirrhosis, diabetes mellitus, and certain occupational exposures (e.g. use of vibration tools or heavy manual work)
Clinical Features
Patients will present at varied stages of disease progression. Symptoms may therefore range from a reduced range of motion and nodular deformity, through to a complete loss of movement.
The ring or little finger are most commonly involved. The right hand is more commonly affected, however the condition is bilateral in 45% of cases.
On examination of the hand, a thickened band (Fig. 2) or firm nodule adherent to the skin may be palpable. Skin blanching may occur on active extension of the affected digits. In advanced disease, the MCP and/or PIP joints of the affected digit may be in contracture.
Hueston’s test is a specific test that can be performed for such patients – if the patient is unable to lay their palm flat on a tabletop, this is a positive test.
Differential Diagnosis
Important differential diagnoses to consider in patients presenting with the condition include stenosing tenosynovitis (often painful and associated with overuse or trauma), ulnar nerve palsy (associated with reduced movement/strength and loss of sensation), or trigger finger (painless locking or clicking finger on flexion).
Investigations
The diagnosis of a Dupuytren’s contracture is a clinical one. Patients can have selected routine blood tests performed, such as a HbA1C test, to assess for potential associated risk factors (as above)
Management
The management is mainly dependent on the stage of presentation. Patients who present early with no functional disability can be monitored and treated with conservative management initially. More invasive treatment can then be considered when there is functional disability or rapidly progressive disease.
Conservative Management
Patients are advised to undergo hand therapy, keeping the hand active with multiple stretching exercises throughout the day.
Injectable collagenase clostridum histolyticum (CCM) is used in select centres in early disease, as data shows that for early stages of Dupuytren’s contracture its use is equivalent to surgery in functional outcomes (albeit with high recurrence rates)
The use of steroid injections is not routinely recommended for early Dupuytren’s disease.
Surgical Management
Surgical procedures for Dupuytren’s disease involve the excision of diseased fascia. Surgical management is typically indicated in those with functional impairment, MCP joint contracture >30 degrees, any PIP contracture, or rapidly progressive disease.
A fasciectomy is the most commonly used surgical procedure for Dupuytren’s disease. These can be performed under local or general anaesthetic, with various possible:
- Regional fasciectomy (most common), whereby the entire cord is removed
- Segmental fasciectomy, whereby only short segments of the cord are removed
- Dermofasciectomy, whereby the cord and overlying skin are removed, to be followed by a skin graft

Figure 3 – Post-operative wound healing following Dupuytren surgery
Closed fasciotomy (also termed percutaneous needle fasciotomy) is a less commonly performed procedure. It has the benefit of being performed in the outpatient setting under local anaesthetic, therefore can be more suitable for co-morbid patients who are unsuitable for major surgery.
The need for a finger amputation is very rare for Dupuytren’s contracture, only ever considered in very severe cases where there has been a delay in presentation and failure of initial management.
Prognosis
The course of the disease is variable and not all disease progresses to contracture. However, most patients will eventually require surgery and, whilst surgical intervention has excellent functional outcomes, post-operative recurrence has been reported up to 66%.
Key Points
- A Dupuytren’s contracture is a common condition involving contraction of the longitudinal palmar fascia
- Main risk factors are smoking, alcoholic liver cirrhosis, and diabetes mellitus
- The ring and little finger are most commonly involved and a thickened band is often palpable on examination
- Surgical management is typically indicated in those with functional impairment, MCP joint contracture > 30 degrees, any PIP contracture, or rapidly progressive disease