Introduction
A hoarse voice refers to a weak or altered voice. It is a relatively common presentation and can represent a wide range of pathologies.
In this article, we shall look at the investigations and differential diagnoses to consider in a patient with a hoarse voice.
The True Vocal Cords
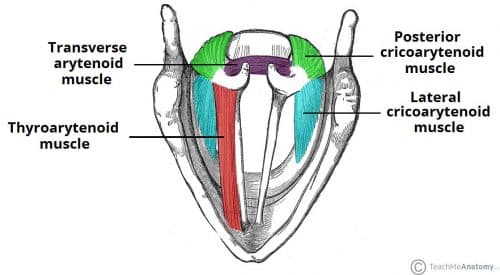
The true vocal cords are responsible for producing voice by being able to abduct and adduct, through innervation from the recurrent laryngeal nerve and the external branch of superior laryngeal nerve.
The recurrent laryngeal nerve supplies all the intrinsic muscles of the larynx, apart from the cricothyroid muscle which is supplied by the external laryngeal nerve. The cricothyroid muscle increases the pitch of our voice.
Any pathology affecting the structure of the vocal cords or their innervation will result in hoarseness.
Investigations
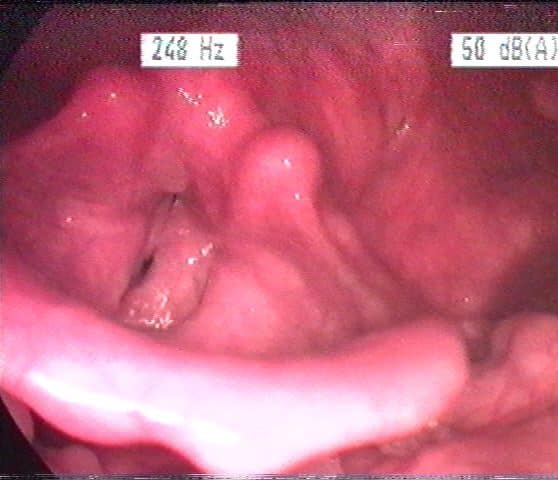
It is essential for any patient presenting with a hoarse voice to undergo a flexible nasal endoscopy (FNE). FNE allows visualisation of the larynx and the vocal cords (Fig. 2), therefore key in identifying any underlying pathology, such as vocal cord palsy or structural abnormality of the larynx. It can be performed in the outpatient clinic, with minimal preparation required.
Microlaryngobronchoscopy (MLB) is another procedure that allows for visualisation of the larynx, vocal cords, and bronchi. It is performed under general anaesthetic in theatres, usually done as an elective procedure. MLB also allows for biopsies or treatment options too, such as microdebridement or laser excisions to be performed.

Figure 2 – Microlaryngoscopy view of the vocal cords (anterior is top of the image)
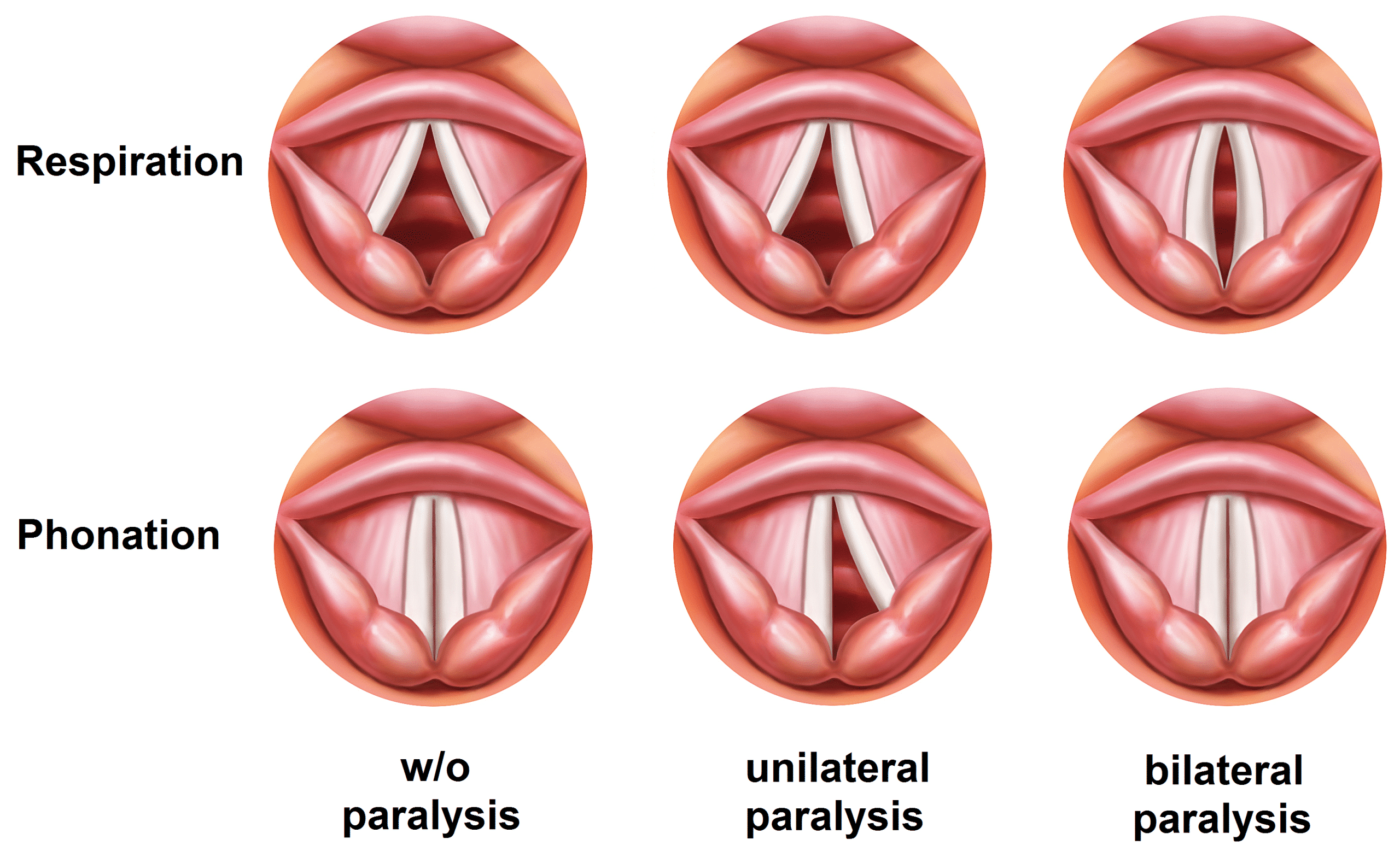
If patients are suspected of having a vocal cord palsy, additional investigations are often required. These can include CT neck and chest (to assess for any lesion along the path of recurrent laryngeal nerve) or laryngeal electromyography (EMG, to distinguish between palsy from fixation, i.e. neural – paralysis, joint – fixation).
Video-stroboscopy is used in specialist voice clinics and can be a useful diagnostic test in vocal cord dysfunction. It involves the use of synchronised flashing lights to make vocal fold movements appear slower, allowing for complete assessment of their movement.
Swallowing assessments such as Flexible Endoscopic Evaluation of Swallowing (FEES) or Video Fluoroscopy (VF) to be done by Speech and Language Therapists (SALT) if there were any concurrent concerns regarding a safe swallow.
Differential Diagnosis
There are a multiple causes of hoarseness, ranging from simple benign conditions to serious malignant or neurological causes. Regardless, all cases of new onset hoarseness need investigation and management depends on the underlying cause. Functional causes should be seen as a diagnosis of exclusion when no obvious cause can be found, however it is a common cause for hoarseness.
Benign Laryngeal Conditions
Vocal Cord Nodules
Vocal cord nodules are commonly secondary to chronic phonotrauma (vocal abuse). They are benign lesions that are frequently bilateral (Fig. 3), occurring at the junction between the anterior and middle third of the vocal folds due to strain. Management is mainly voice therapy from the SALT team, however in severe or resistant cases, surgical intervention may be warranted
Intercordal Cysts
Intercordal cysts (or vocal cord cysts, Fig. 4) can be due to phonotrauma or blockage of mucous gland excretory duct. They are usually investigated with videostroboscopy and are typically managed conservatively with voice therapy from the SALT team. If persistent, cysts can be excised with microdebrider or CO2 laser.
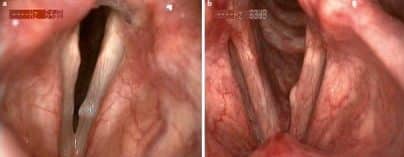
Figure 4 – Flexible nasal endoscopy showing a vocal fold cyst (left) and scarring from a vocal fold cyst (right)
Muscle Tension Dysphonia
Muscle tension dysphonia is caused by habitual misuse of the muscles of the larynx. It commonly presents with a hoarse voice that worsens towards the end of the day or following prolonged use. Diagnosis can be confirmed via stroboscopy and the mainstay of management is voice therapy from the SALT team
Vocal Cord Polyps
Vocal cord polyps are typically benign lesions (Fig. 5), however unlike vocal cord nodules, they are normally unilateral and may need surgical excision to exclude malignancy.
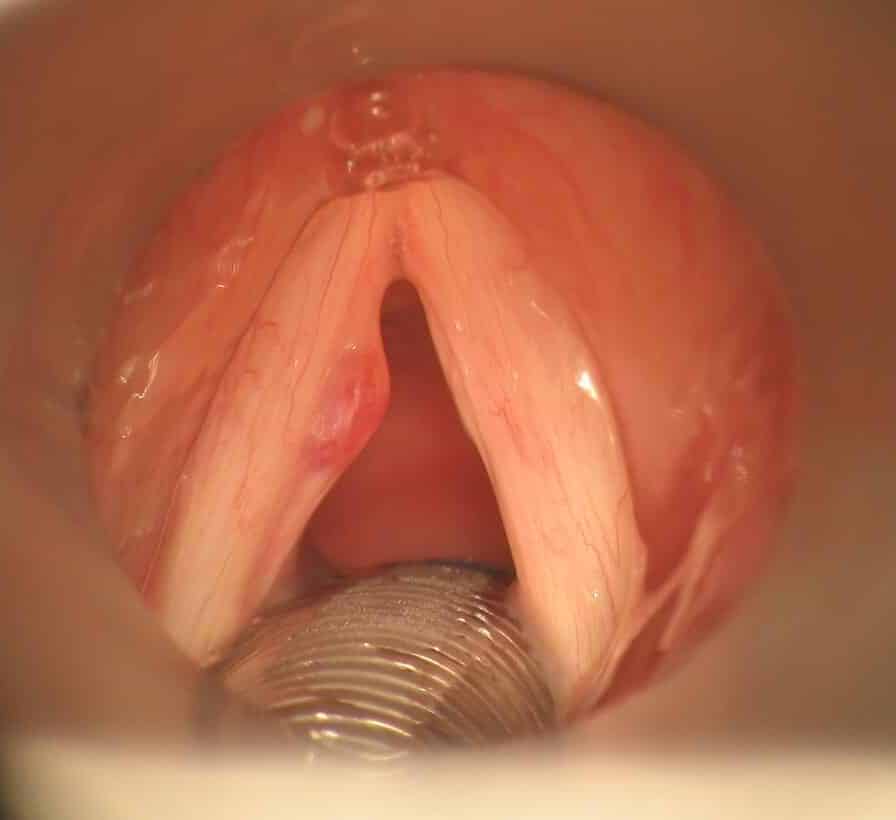
Figure 5 – Microlaryngoscopy view of a vocal cord polyp
Laryngeal Papillomas
Laryngeal papillomas are benign lesions in the larynx, commonly caused by HPV infection. If left untreated, papillomas can grow to cause airway obstruction and hence need surgical excision or debulking. It is not uncommon for patients to need repeat procedures as papillomas can recur.
Laryngopharyngeal Reflux
Laryngopharyngeal reflux (LPR) is a caused by acid reflux resulting in inflammation of the larynx. Whilst clinical examination will often be unremarkable, but FNE will reveal interarytenoid oedema, oedematous vocal cords, or granulations of the vocal cord process. Further investigation may require an gastroscopy and treatment will be with proton pump inhibitor (PPI) therapy ± H. Pylori eradication therapy.
Reinke’s Oedema
Reinke’s oedema is oedema of the vocal folds (Fig. 6). It is strongly linked to smoking and is more common females, but can also be seen with laryngopharyngeal reflux. Smoking cessation and voice therapy are the mainstay of treatment.

Figure 6 – Flexible nasal endoscopy view of oedematous vocal cords, as seen in Reinke’s oedema
Infective
Laryngitis
Laryngitis is inflammation of the vocal cords, commonly following respiratory tract infections. Clinical examination will be normal, however FNE will reveal an acutely inflamed larynx (Fig. 7). This can be managed conservatively and should result in complete recovery.
Supraglottitis and Epiglotittis
Supraglottitis is inflammation of the supraglottic structures, commonly after respiratory tract infections. FNE findings may show oedematous arytenoids and mildly inflamed epiglottis. These are usually treated with antibiotics and should result in complete recovery.
Acute epiglottitis is infection of the epiglottis, further discussed here.
Malignancy
Laryngeal cancers are usually squamous cell carcinomas (SCC), associated with human papilloma virus (HPV) infection. It can be further classified into supraglottic, glottic or subglottic in origin.
Patients present with a hoarse voice, alongside potential other red flag signs such as a neck lump, dysphagia, weight loss or referred otalgia. Investigation and management options are further discussed here.
Neurological
A recurrent laryngeal nerve palsy can be caused by a wide range of causes, including thyroid cancer, lung cancer, thoracic aortic aneurysm, multiple sclerosis (MS), or stroke.
Extensive examinations are key to further delineating the underlying diagnosis, including neck examination and cranial nerve examination. Most cases would warrant CT imaging from skull base to diaphragm, to assess for any pathology affecting the recurrent laryngeal nerve route.
Key Points
- A wide range of pathology can result in hoarseness, from inflammatory to neurological
- All patients should undergo flexible nasal endoscopy to allow for the visualisation of the larynx and the vocal cords, before subsequent further investigations