Introduction
Small bowel tumours are rare, accounting for <5% of all gastrointestinal cancers, despite the small intestine contains over 90% of the mucosal surface area of the gastrointestinal tract. In the UK, their incidence is around 2-3 cases per 100,000 population per year.
Most small bowel tumours arise from the duodenum (around 55-80% of cases), and less commonly arise from the jejunum (10-25%) or ileum (5-15%).
Small bowel neoplasms can be either benign or malignant:
- Benigntumours – typically adenomas, subclassified as simple villous, tubular, or Brunner’s gland adenomas; less common types are leiomyomas, lipomas, and desmoid tumours
- Malignanttumours – most common types are either adenocarcinomas or neuroendocrine tumours (40% respectively*), with less common types being stromal tumours, sarcomas, and lymphomas
For small bowel adenocarcinoma, the average age of diagnosis is 66yrs (lower than the colorectal cancer average), with equal incidence between men and women
*Adenocarcinomas more commonly affect the duodenum whilst neuroendocrine tumours more commonly affect the ileum
Pathophysiology
Small bowel adenocarcinomas are believed to arise from pre-existing adenomas through a sequential accumulation of genetic abnormalities (a model similar to that described for the pathogenesis of colorectal cancer), which can occur over several years.
The tumour suppressor gene p53, which maintains DNA integrity, and the oncogene KRAS, which normally functions in cellular signalling and proliferation, have been implicated in over 50% of small bowel adenocarcinoma cases.
Risk Factors
Non-modifiable risk factors for small bowel adenocarcinomas include increasing age, Crohn’s disease or coeliac disease, and certain genetic conditions (such as Peutz-Jeghers syndrome, Lynch syndrome, or familial adenomatous polyposis).
Modifiable risk factors for small bowel adenocarcinomas include smoking, obesity, low fibre intake, high intake of red meats, and alcohol excess.
Clinical Features
Most small bowel tumours are initially asymptomatic. However, as they increase in size, they most commonly become symptomatic by causing small bowel obstruction (or a gastric outlet obstruction if proximal) due to luminal narrowing (or rarely through intussusception). Less commonly, they can present with PR bleeding (either as fresh PR bleeding or melena, depending on their location)
On examination, an abdominal mass may be palpable in around 25% of cases. In those presenting with metastatic disease, this can also present with cachexia, jaundice, hepatomegaly, or ascites. Neuroendocrine tumours can also present with carcinoid syndrome.
Investigations
Due to the absence of symptoms or non-specific presentations associated with most small bowel neoplasms, such cancers are rarely diagnosed in the outpatient setting.
Blood tests are also non-specific for small bowel tumours. Elevated carcinoembryonic antigen (CEA) levels are associated with small-intestinal adenocarcinomas, however only in the presence of liver metastases, whilst elevated serum 5-hydroxyindole acetic acid (5-HIAA) levels is only observed in certain patients with carcinoid syndrome.
Imaging
For proximal duodenal small bowel tumours, an upper GI endoscopy can be performed (Fig. 4), also allowing for histological sample to be obtained via biopsy.
However, often endoscopy cannot reach the suspected tumour, therefore in such cases, MRI enterography can be used to good effect in the diagnosis. Other imaging modalities that can be used include endoscopic ultrasound (EUS) (especially for cancers in the ampullary region) or capsule endoscopy.
However, as the majority of patients present with features of bowel obstruction, often the diagnosis (or suspicion raised) is made via CT imaging, especially if the tumour is large. Further PET-CT imaging is useful if metastatic disease is suspected. Small bowel tumours are staged using the TNM staging system.
Management
Any symptomatic benign small bowel tumour should be resected if feasible, either endoscopically or surgically. Choice of intervention depends on patient factors, size and location of the tumour, and subtype of the tumour
Neoadjuvant chemotherapy or chemoradiotherapy* may be needed for some locally advanced disease, prior to any surgical intervention.
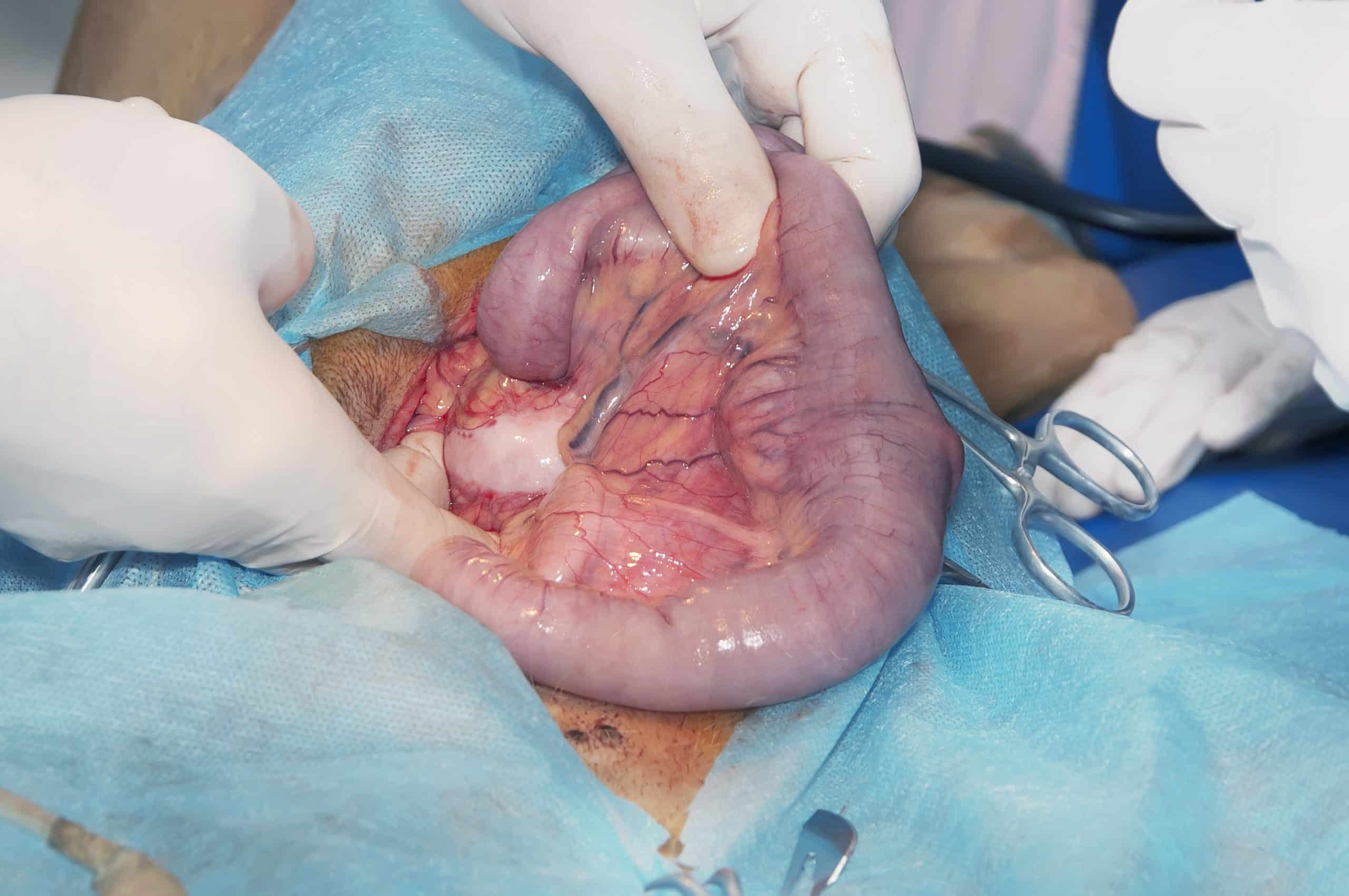
For local small bowel adenocarcinomas, surgical resection is the only definitive treatment. The type of resection used depends predominantly on the location of the tumour; segmental resection of the small bowel is often the mainstay of treatment, although duodenal tumours may require either pancreaticoduodenectomy (Whipple’s procedure) or segmental duodenal resection.
Adjuvant chemotherapy is likely required for lymph node positive disease (often with a similar protocol as colorectal cancers). Management of neuroendocrine tumours is discussed further here.
*GISTs expressing exon 9 and 11 KIT mutations can also receive imatinib as neoadjuvant/adjuvant therapy.
Metastatic Disease
Approximately 35% of patients diagnosed with small bowel adenocarcinoma have stage IV disease (distant metastatic) at presentation. Choice of chemotherapy regime is guided by patient factors and function – systemic therapy options include fluoropyrimidine-based chemotherapy, taxane-based chemotherapy, or checkpoint inhibitors.
Prognosis
At the time of diagnosis, around 70% of patients with a small bowel adenocarcinoma have potentially resectable disease. The 5-year survival for node-positive small bowel adenocarcinoma is between 12-50%.
Key Points
- Small bowel tumours are rare, accounting for <5% of all gastrointestinal cancers
- Most common benign types are adenomas and the most common malignant types are adenocarcinoma and neuroendocrine tumours
- The most common presentation for small bowel tumours is with clinical features of bowel obstruction
- Where feasible, all small bowel tumours need resection, either endoscopically or surgically